Antibiotics are NOT Chicken SoupWe are all familiar with the expression “Chicken soup…may not help but wouldn’t hurt”. Endodontists have become alarmed with the tendency for referring dentists to prescribe antibiotics, like chicken soup, without understanding their proper usage. It is understandable that clinicians wish to provide relief for their symptomatic emergency patients with the least interruption of their practice day. However, wholesale use of antibiotic prescriptions, as an effortless method of “getting the patient out of the office” or “dealing with the symptomatic telephone call” must be condemned. Understanding pulp pathology precludes use of antibiotic therapy in vital cases. It is ironic that clinicians who prescribe antibiotics for thermally sensitive “sick pulps”, do not recognize that part of the pathology involves compromise of circulation to this organ. Antibiotic therapy is of NO value in the case of pulpitis with a vital pulp. Antibiotics rely on the attainment of an adequate concentration of the medication via the circulation. With circulation compromised by inflammation, there is no way for this medication to reach the affected area i.e./ the most coronal or radicular pulp. The most critical management decision facing the clinician dealing with an emergency pulpitis, is whether or not periapical symptoms are present. The Thermally Sensitive Tooth with NO Periapical Symptoms The problem is the coronal pulp. Treatment is pulpotomy (or pulpectomy if there is sufficient time). This will relieve the thermal symptoms and allow the patient to be rescheduled for completion of endodontic treatment when time allows. Antibiotics are contraindicated. The Periapically Involved Tooth Teeth with periapical involvement will have signs that include percussive sensitivity, periapical palpation sensitivity and/or swelling and sometimes visible radiographic periapical pathology. Relief will be most predictably obtained by pulpectomy. Canals should be broached, irrigated and cleaned to approximately size #15 or #20 instrument (if possible) with electronic confirmation of working length. In this way, the minimal remaining pulp remnants have little possibility of increasing the periapical inflammation. The occlusion is relieved and the patient is placed on anti-inflammatory medication. Antibiotics are rarely required. Routine prescription of antibiotics “just in case”, is not supported by the literature. Post Treatment Exacerbation – (Blow Up) In rare cases, you may need to place the patient on antibiotics if they develop post pulpectomy blow up. This usually occurs 48 hours after treatment and is due to pushing debris out of the apex. It is more often associated with necrotic or retreatment cases. Pathology is due to inoculation of the periapical area with pulp content and bacteria, inadvertently introduced into this area by a file. When placing instruments in canals, working lengths must be accurate. Use an apex locator to prevent being long with files. Confirm working lengths with images (x-ray film or digital radiography). If the case blows up, there will be PDL inflammation. The tooth will extrude and periapical palpation sensitivity and swelling will occur. The first 48 hours post-treatment are the most critical. Good communication follow-ups by staff-members prevent cases from getting out of control. Antibiotics should be given in those cases where swelling is reported. It is important to start the medication early and to ensure that the patient does NOT apply heat to the area externally. THERE IS NO SCIENTIFIC BASIS FOR GIVING ANTIBIOTICS AS A “PROPHYLAXIS” IN THE CASE OF THE SINGLE APPOINTMENT TREATMENT OF A NECROTIC TOOTH. Clinicians considering Antibiotic therapy should read :
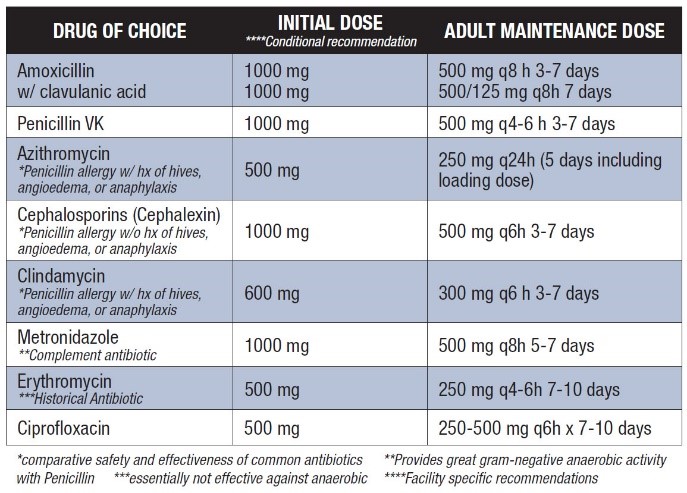
AAE Fall 2019 ENDODONTICS: (To Download Click Here – AAE Antibiotics 2019 Update) This article categorizes various antibiotics used in treatment as well as indications for their use. Here is a chart from that article (2019 update) |
|
In the best case scenario, the continued irrational use of antibiotics as “do something” treatment, contributes to the proliferation of antibiotic resistance. The consequences will probably not be apparent to clinicians in their middle or late career years. The problem will no doubt escalate in the future, as bacteria become more resistant and we are left with fewer effective drugs. Those of us prescribing in a haphazard manner may well be responsible for a situation where our children and grandchildren have fewer and fewer alternatives for treating serious bacterial infection in other, more critical areas of the body. In the worse case scenario, a patient may undergo an anaphylactic reaction, possibly resulting in death. The chances of this happening are remote. But should that happen to your patient, and you are required to justify your prescription in a court of law, do you want an Endodontist to be forced to tell the court that your prescription was not indicated, ineffective and unsupported by any of the literature? Responsible use of antibiotic therapy is part of good dental practice. Clinicians who are unwilling to take the time to properly diagnose and treat a problem or who are not able to make a definitive diagnosis should opt for referral. The use of antibiotics as scattergun treatment for problems of unknown etiology is poor clinical practice. Antibiotics are not “chicken soup” and clinicians should not use them in this manner. They should not be used as a “Do something – dismissal tool” when you are too busy or are unable to make a diagnosis. When in doubt, refer the case to a specialist.
|