Failing Anterior NSRCT needs SRCT
A 68 year old female patient in good health was referred to my office for consideration of tooth #21. The patient’s current complaint was a history of previous intermittent swelling in the buccal vestibule and sensitivity to percussion. The patient had the problem for approximately two weeks and had been seen by her regular dentist, who made endodontic access of the tooth.

Figure 1: Preop image
Prior access of tooth #21 by referring dentist snad associated large periapcial radiolucent finding.

Figure 2: Preop image of maxilla
Very healthy gingiva. Hygiene excellent. Good candidate for surgery. I noted notch and discoloration in previously treated #11.
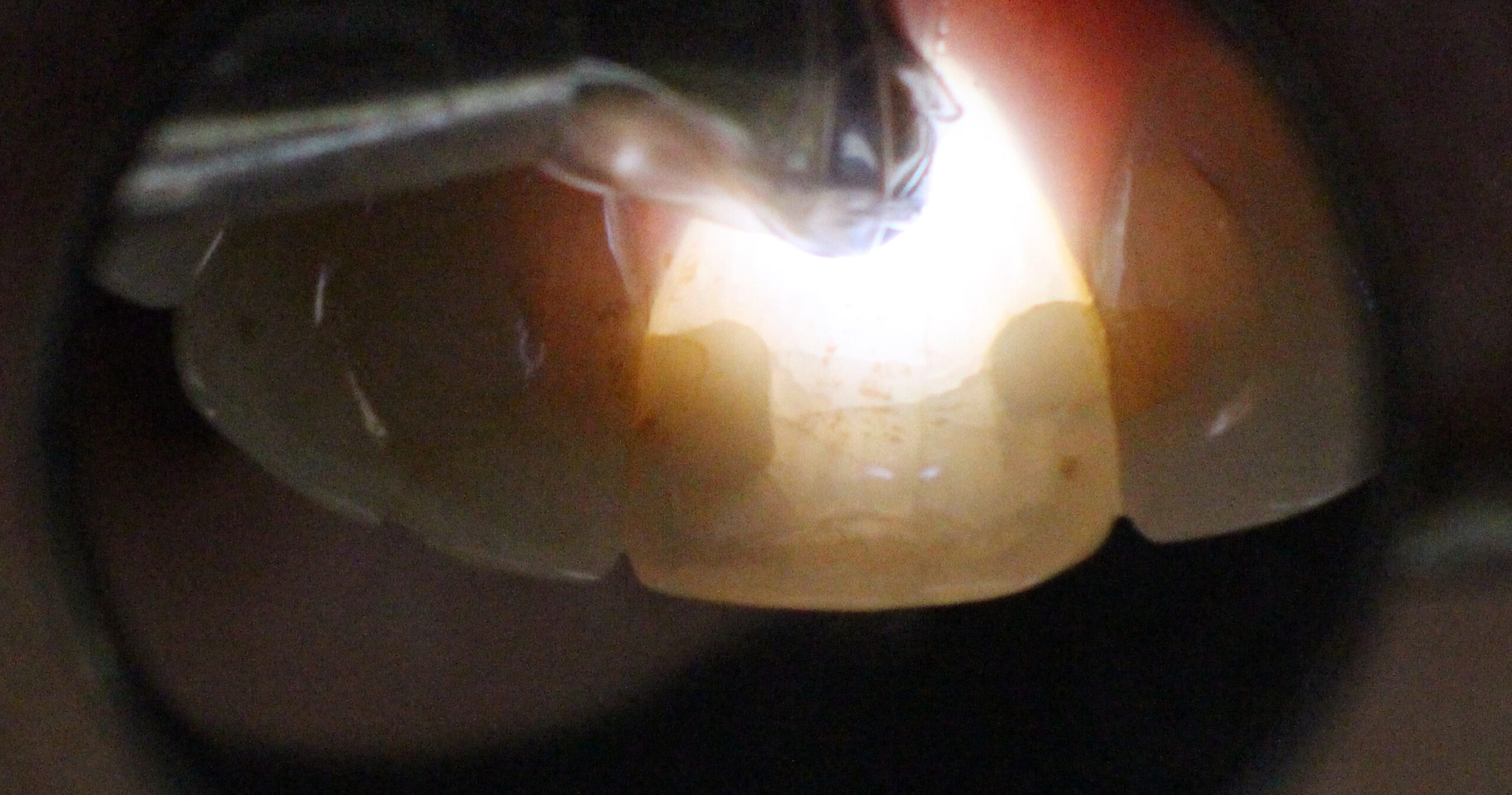
Figure 3: Palatal transilluminatoin of #21
Transillumination showed crack running in between the 2 x Cl 3 M and D restorations. While this MAY not be initially significant, making endodontic access through this area on the palatal side can only contribute to weakening the crown in this area and serve as a nidus for future possible fracture of the crown. The patient needs to be informed of this prior to access. Transillumination should always be part of a complete endodontic examination.
Pulp tests performed on the adjacent lateral incisor showed positive responses, indicating normal pulp vitality. #11 had been previously endo treated and apparently had internal bleaching procedures performed without proper sealing of the coronal part of the canal, which was still unfilled. #11 was still discolored ( and chipped) and the patient was unhappy with the clinical appearance. Perio findings in #s 11, 21 and 22 were WNL but buccal palpation sensitivity over #21 was confirmed.

Figure 4: Ca(OH)2 Medication
The canal system in #21 has been cleaned, shaped and medicated. We now wait for symptoms to subside and for us to be able to dry teh canal sufficiently to allow for eventual obturation.
Treatment of #21 was initiated. The canal was cleaned, shaped and medicated with Ca(OH)2. The medication would be left until the patient was asymptomatic and the canal could be adequately dried. The canal was subsequently obturated and closed with a matching palatal composite.
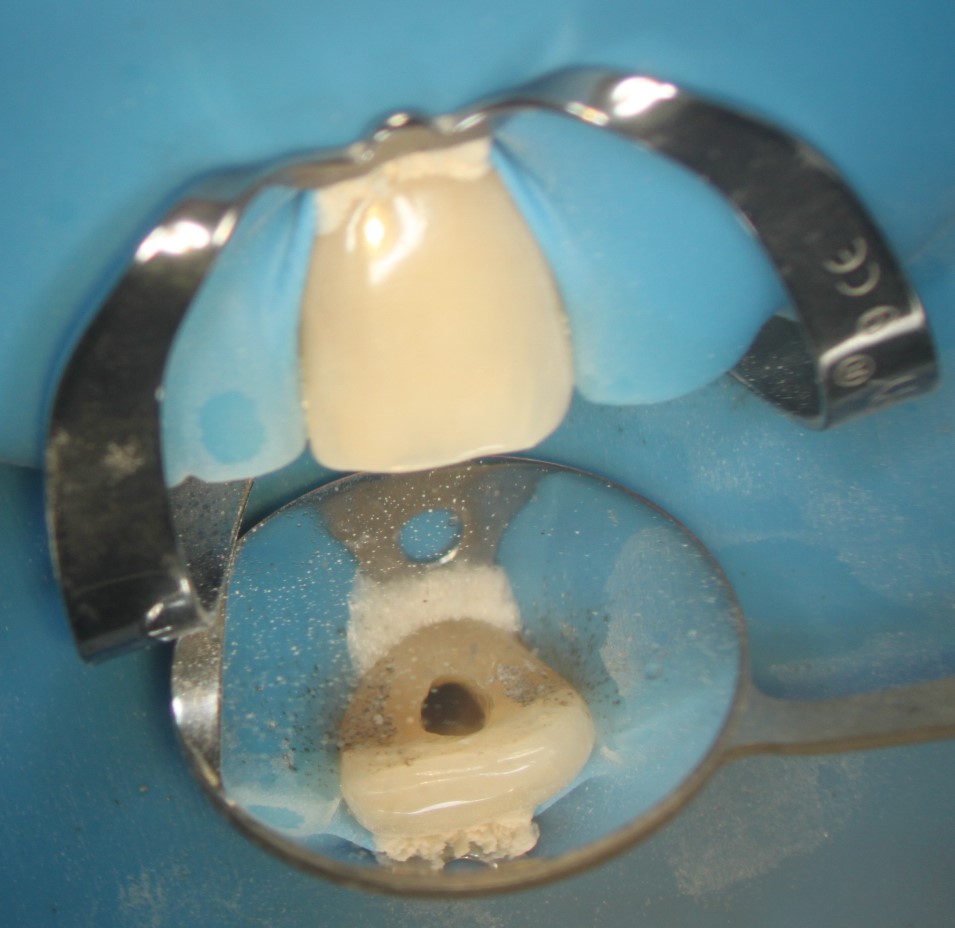

Figure 5: Obturation of the canal
The access is immediately closed with a permanent restoration. In this case it is a bonded composite.

Figure 6: Preop image
Prior access of tooth #21 by referring dentist snad associated large periapcial radiolucent finding.


For reasons that were unclear to me, the patient eventually ended up in another Dentist’s office. ( From the Spanish notation above the image, this may have been on vacation or “Dental Tourism”.) In any case, the Dentist probably saw the radiolucent area and assumed that it was coming from #22. ( Had he performed a pulp test, he would have found the pulp to be responsive and normal.) Therefore, the tooth was treated unnecessarily and the endo treatment was not therapeutic for the patient.
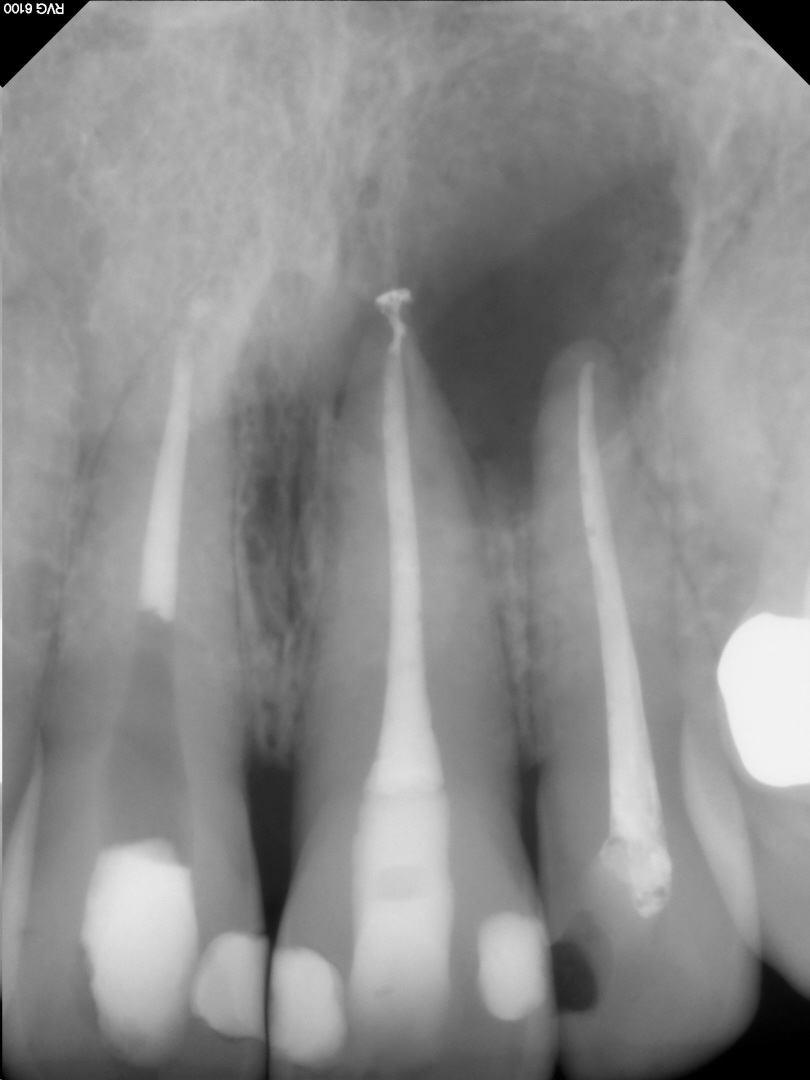
Figure 7: Pre-Surgical image
The area continued to be a source of discomfort and even though the endodontic treatment appeared good radiographically, we needed to address the problems surgically.
cbCT imaging showed that the periapical radiolucent area involved the apices of BOTH #21 and 22. So, if were were to perform apical surgical procedures on #21, (surgically enucleating the entire lesion) it would have also likely required elective endodontic treatment of #22. Otherwise, there was a high likelihood that removal of the tissue would have severed the apical vasculature supply to #22, requiring subsequent NSRCT. In situations such as this, it is sometimes preferable to do elective NSRCT of the adjacent tooth BEFORE the surgery to prevent possible necrotic pulp products in #22 from compromising healing of the area. In this case, treatment of #22 had already been performed.
cbCT imaging also showed that the radiolucent finding did NOT involve the palatal plate and therefore was not a true “thru and thru”. The chances of healing without the need for GTR or barrier placement were excellent because of this finding.

BU flap with elevation and exposure of the roots of #22 and 21. The lesion was enucleated in its entirelty and placed in Formalin for biopsy analysis.
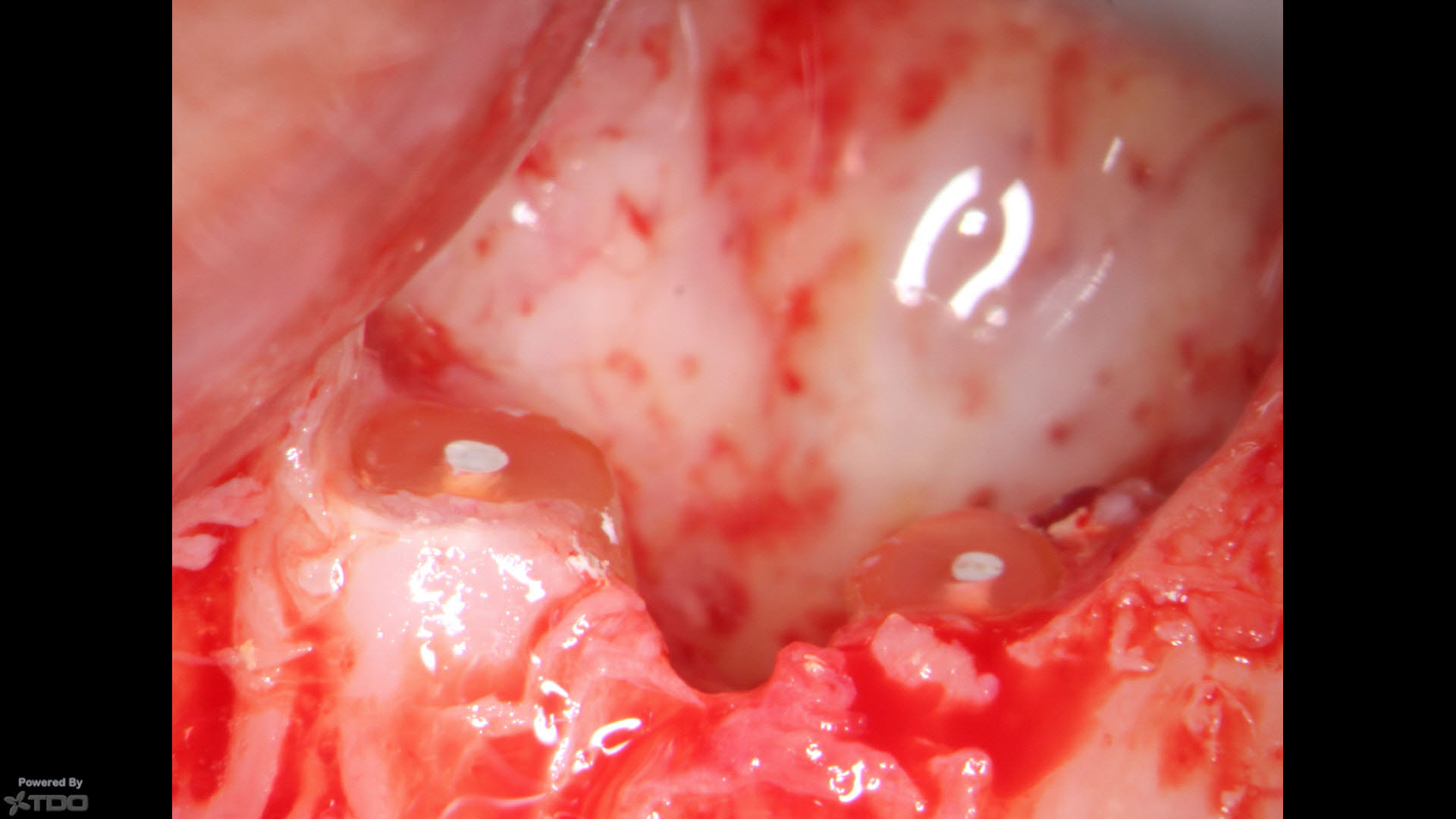
Removal of the lesion allowed for excellent hemostasis and access to the root ends. No”Apical Plaque” was visible and the roots were resected to the level of the adjacent normal bone, retro-prepared with ultrasonics and filled with MTA putty.

The area was sutured with 6/0 Proline with an effort made to keep the knots OFF the suture line. It has been my experience that this results in better, quicker healing.
Biopsy Report returned with a finding of Periapical Granuloma.

Figure 8: Post-op image
Both teeth resected and retrofilled. No bone grafting material or barriers were placed.

4 day postop suture removal. The patient’s post op care and hygiene have resulted in excellent soft tissue healing.
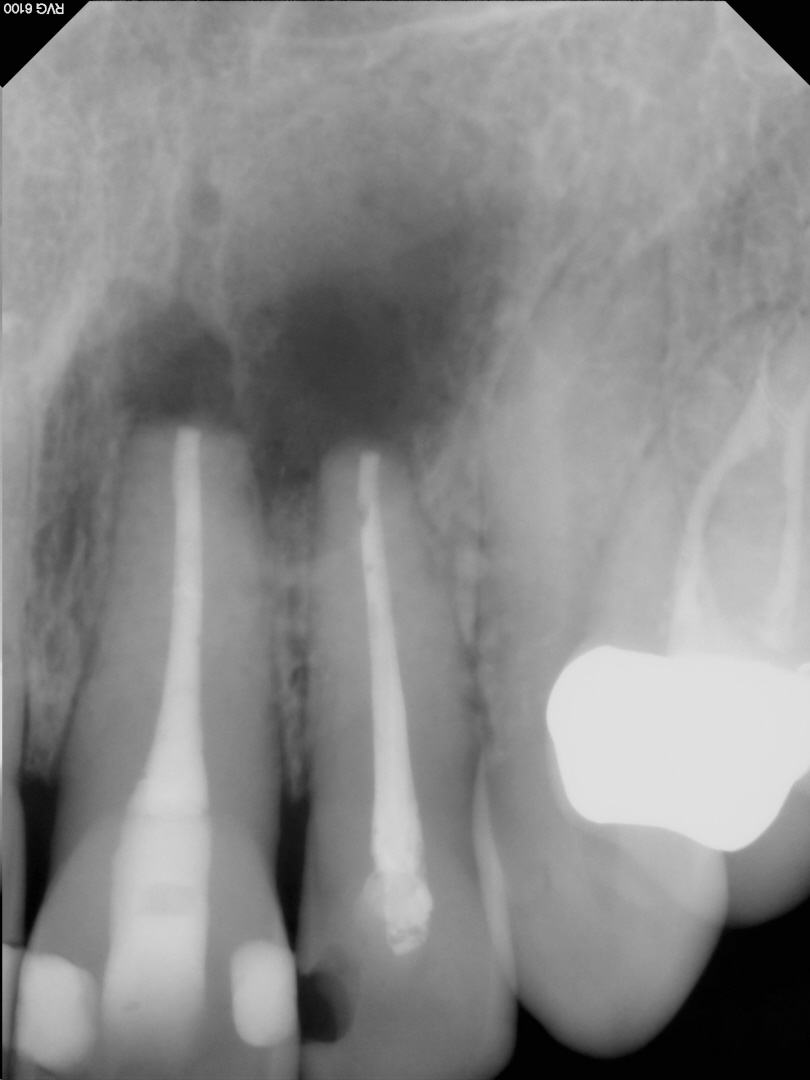
Figure 9: 1 year recall image. Bone fill proceeding slowly.
Patient asymptomatic.
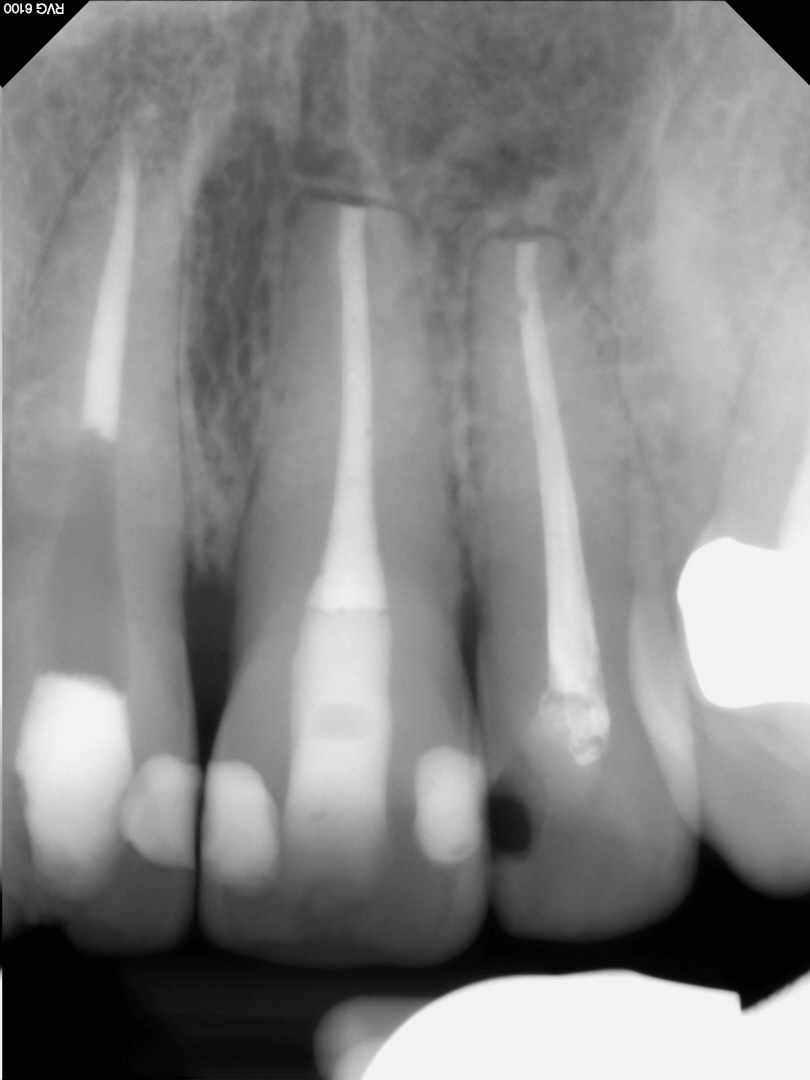
Figure 10: 2 year recall image
Bone completely filled in.

Figure 11: 2 year Recall image
Excellent soft tissue result. No scarring and nice clinical healing overall.
Unfortunately the situation with previously Endo treated #11 has never been addressed!! The incisal chip is now larger.