Post Placement and Occlusion Affect Prognosis
A 59 year old male patient was referred to me for consultation regarding symptoms associated with tooth #14. The tooth had been endodontically treated and restored some years earlier. The tooth was restored with a 2 post retained crown and crown. The patient’s current complaint was a low grade sensitivity to chewing and soreness in the gingival area.

Figure1 : Crown restoration of #14
The patient had a porcelain bonded to metal crown placed on the first premolar. Other teeth in the quadrant were in good condition.
Clinical examination showed porcelain bonded to metal crown with some gingival redness along the distal marginal gingiva. Buccal Palpation was WNL. Percussion and chewing were positive.
Examination of the periodontium revealed a 10 mm probing depth along the distal side of the root.
Figure 2: Buccal view
No occlusion posterior to #45. #46 and 47 have been lost.

Radiographic examination of the BW and PA images was revealing.
Firstly, I noticed that tooth #46 had been fairly recently extracted since there was still an outline of the root in the mandibular bone. Secondly, I noted that the patient’s maxillary posterior dentition was intact. Both first and second molars were present and although were minimally restored. The supporting Periodontium in these teeth appears to be quite good, However, due to loss of the mandibular first and second molars, these teeth were unopposed.
Figure3 : Periapical image
The patient had both maxillary molars and these teeth were in good condition both restoratively and periodontally. A lateral radiolucent area was noted on the distal aspect of the first premolar at the apical third, coincident with the most apical length of post placement area of

Figure4 : Bite wing radiography
I noted that #16 was unopposed and that #14 appeared to be slightly supra-erupted. The contact between #s 44 and 45 had opened, allowing #14 to drift occlusally into hyper-occlusion.
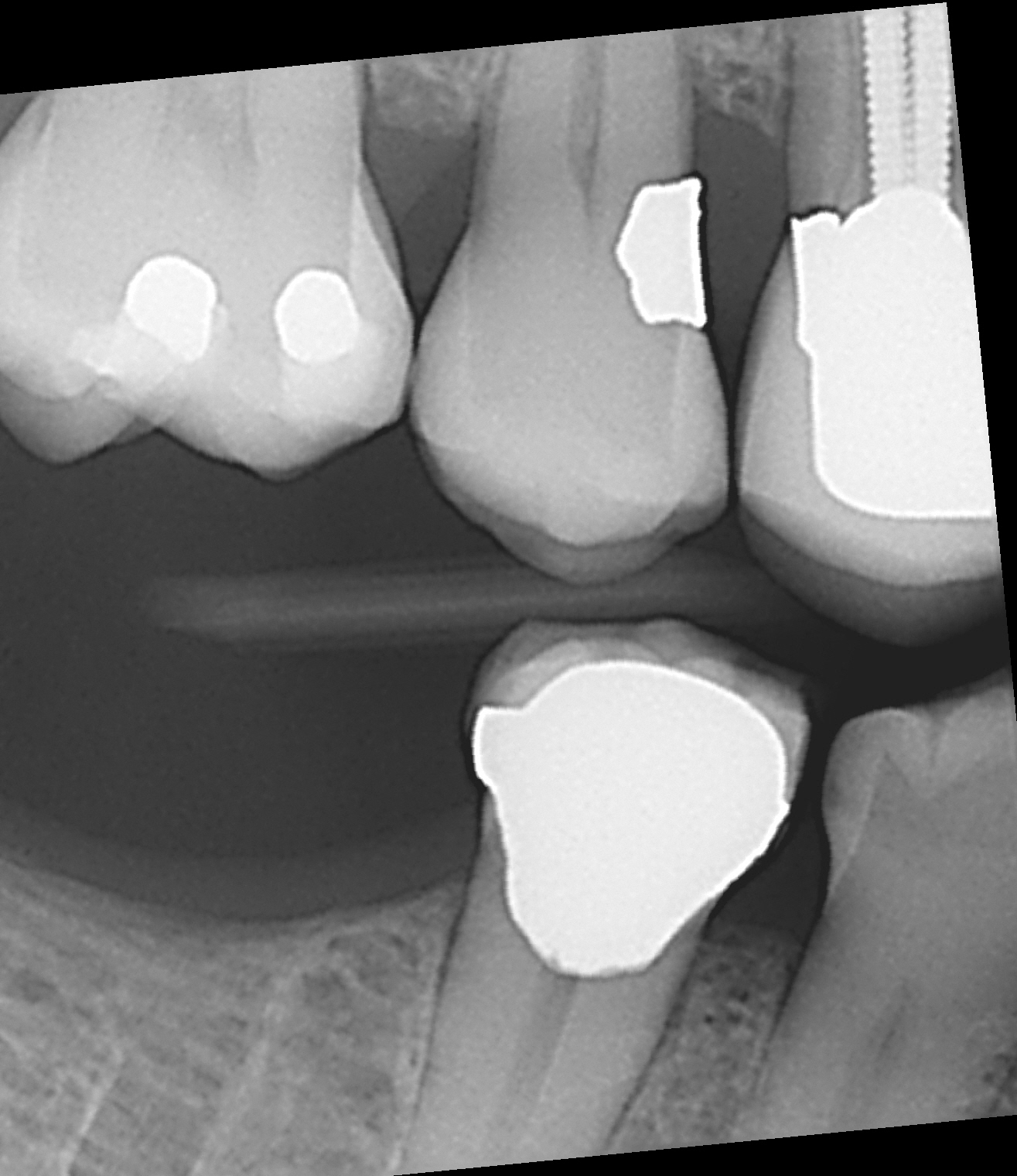
Examination of the occlusal plane showed slight supra eruption of the crown in #14, which appeared to lock into the area between #44 and #45. I surmised that the supra-eruption had occurred partly because of the distal drifting of #45 and open contact that was occurring between #s 44 and 45.
Periapical radiography of #14 showed a crack in the dentin , running from the most apical portion of the post placement, apically. There was an associated lateral radiolucent finding that was consistent with the 10 mm D pocketing.
Figure 5: Root Fracture
It was interesting to note the fracture pattern and that the fact that this tooth had 2 posts placed in it.
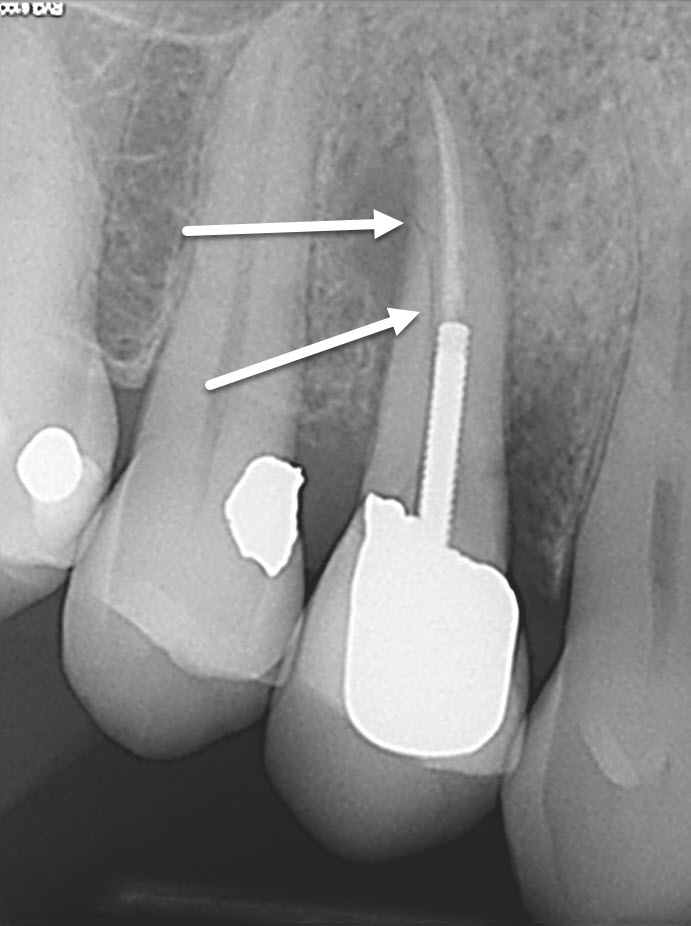
A diagnosis of cracked root was made and the patient was told that the tooth required extraction and prosthetic replacement. We emphasized that the lack of first molar occlusion in the mandible may have contributed to loss of this premolar and recommended that both #14 and 46 be replaced prosthetically ( preferably with implants.)
Although the endodontic treatment of #14 appeared to be good, the method of reconstruction ( using 2 posts rather than a single post), the supra-eruption of the tooth and the lack of posterior occlusion probably all contributed to loss of the tooth.
Endodontic failures can occur, even with good endodontic technique. The clinician endodontically treating the tooth will always depend on proper treatment planning, occlusion and reconstructive techniques if we are to ensure that the endodontic investment is preserved in the long term. Violation of sound restorative principles, ignoring occlusion, and placing teeth under abnormal stress can only contribute to physical failure of the tooth and ultimate loss of even the best Endo-treated cases.
