Handling an Ugly Perforation
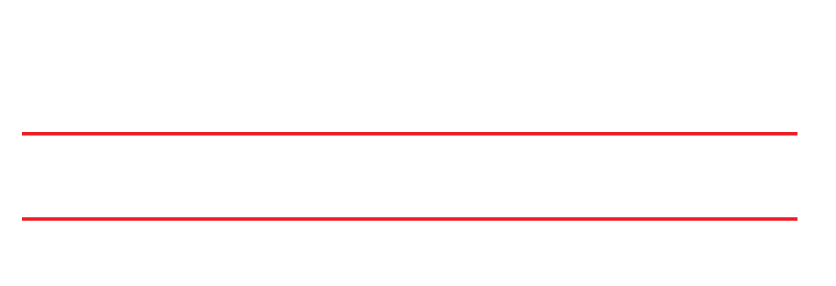
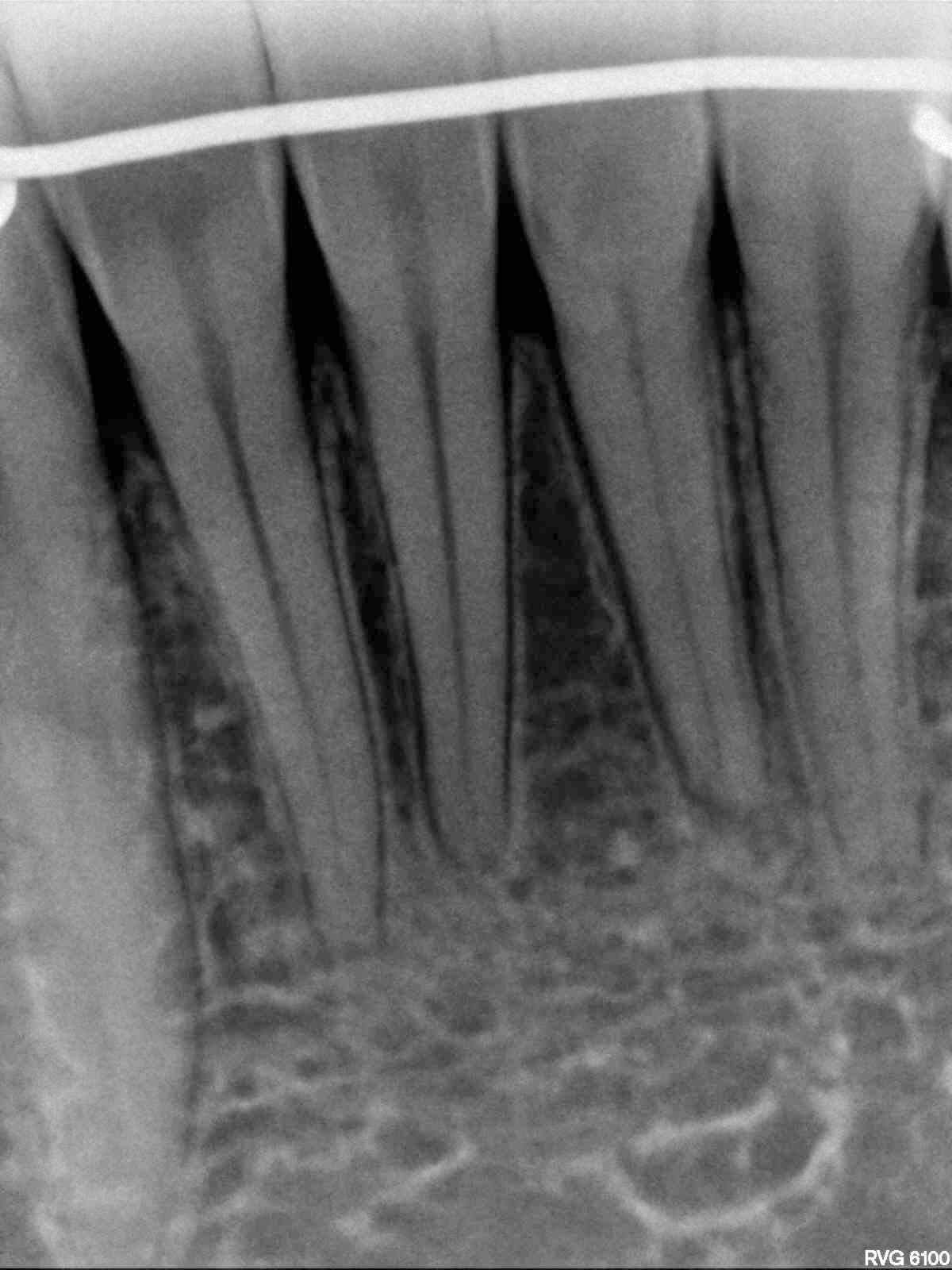
This 29 year old male patient was referred to me in mid treatment. The patient had complained of slight discoloration of this lower incisor and the referring dentist wished to perform an internal bleaching procedure after Endodontic treatment had been performed. Access was made and during the initial entrance into the tooth a labial perforation of the root was made. This remained undetected during the entire instrumentation procedure and eventually the dentist realized that the cone fit was not proceeding normally. The Dentist removed the rubber dam and was alarmed to find a large area of ulceration along the labial gingiva where the instrument had perforated and the irrigation with NaOCl into the gingiva had resulted in tissue necrosis due to what essentially was a chemical burn.

The Dentist explained the procedural error to the patient and referred the patient to me for continuation of the endodontics. I noted that the tooth was virgin prior to access but had slight discoloration . The lingual access had been closed with IRM.
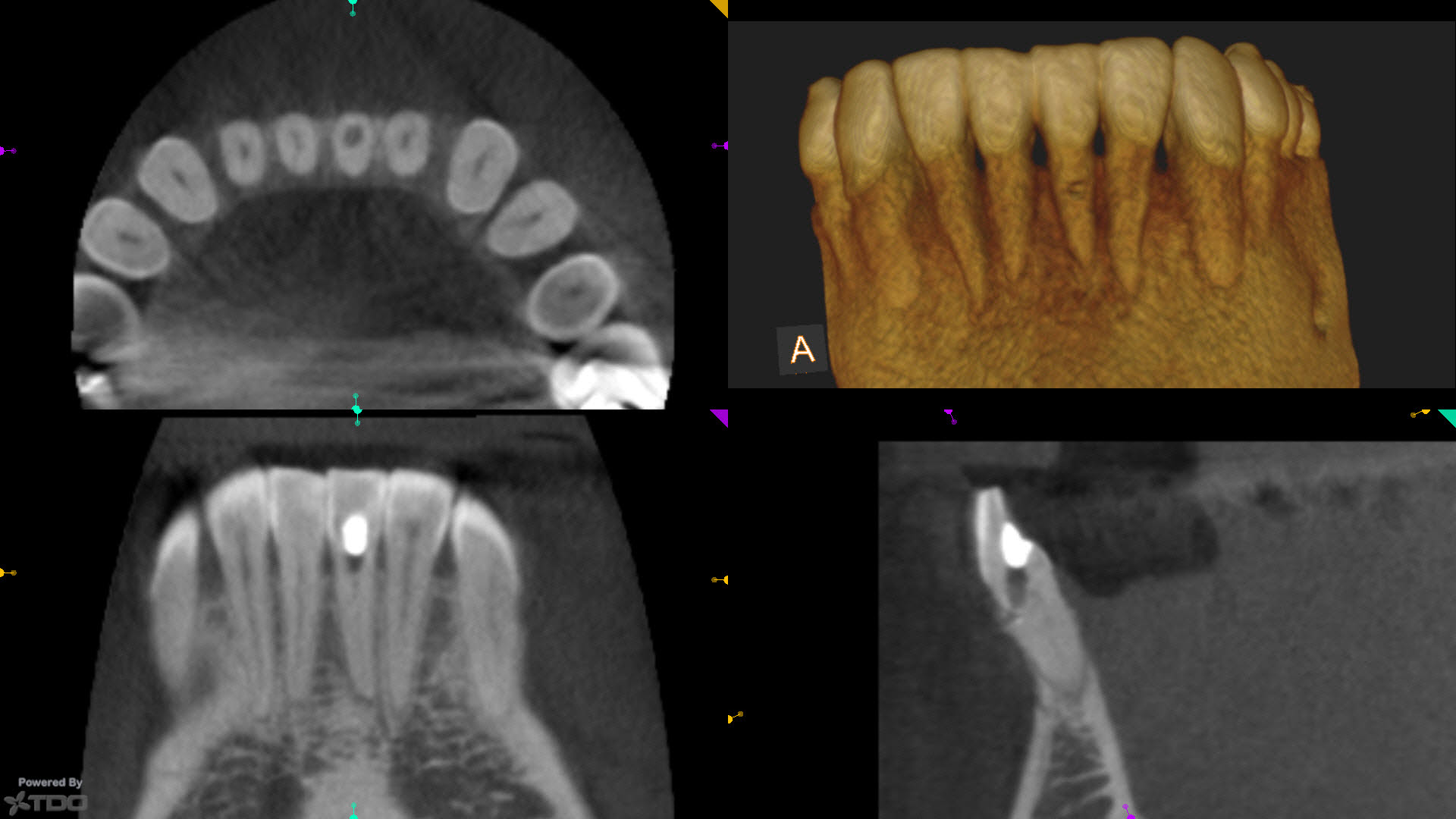
The patient arrived with a large ulcerated area on the labial aspect of the root . Cone beam tomography revealed the perforation site quite clearly . Interestingly, there was no periapical pathology associated with the apex of the tooth in the PA image. So I assumed that this tooth had been electively treated because of lack of pulp responses to pulp tests or perhaps only to allow for placement o internal bleach. The cbCT revealed only a small thickening of the PDL and a bit of resorption at the apex. The tooth was otherwise asymptomatic prior to treatment, as far as the patient had been concerned .

I explained to the patient that there had been a perforation on the labial aspect of the root and that I would attempt to repair this area. I could not guarantee that we could continue with completion of endodontic treatment of the rest of the canal, which I felt may not actually be necessary . It was possible that we could merely fill the perforated coronal section and leave the apical section alone, as long as the patient had no postop symptoms or evidence of periapical radiolucent findings.
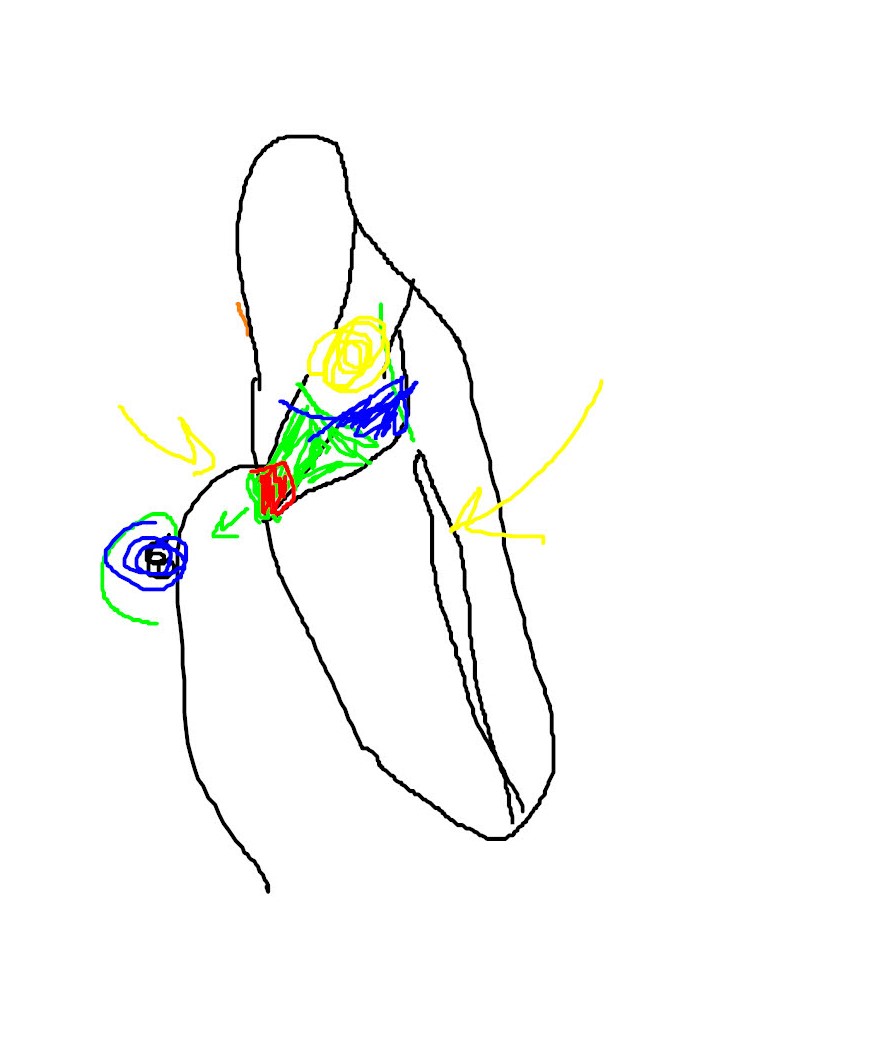
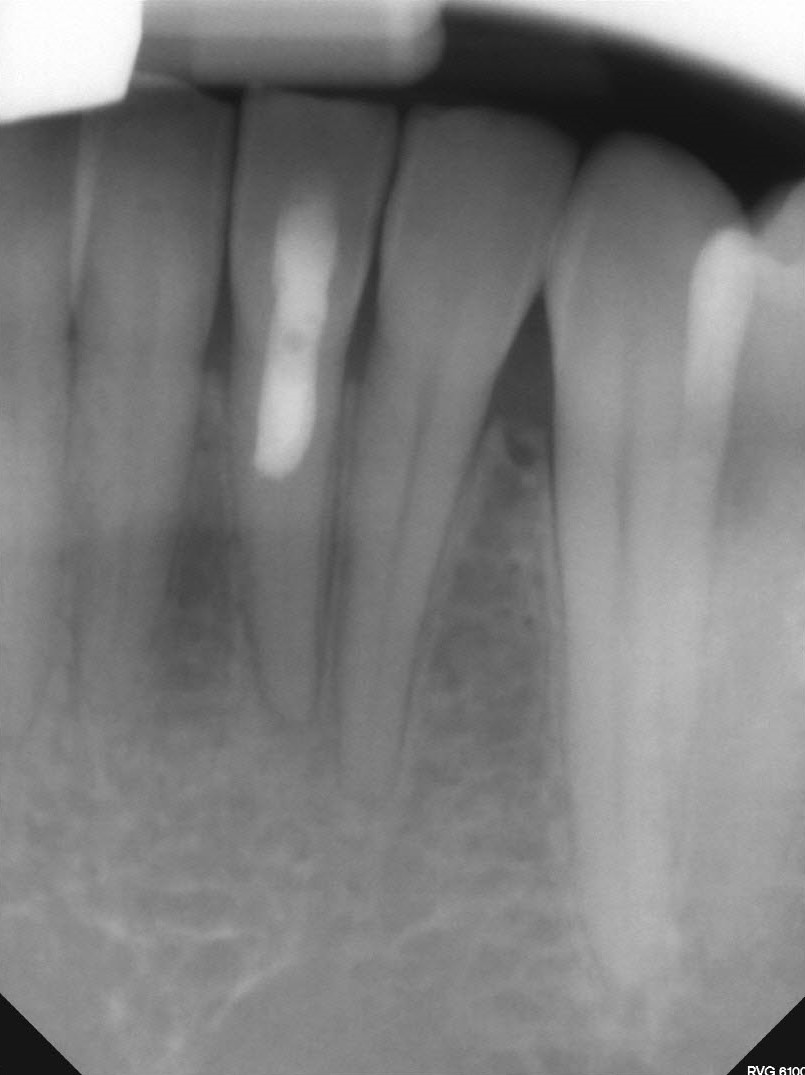
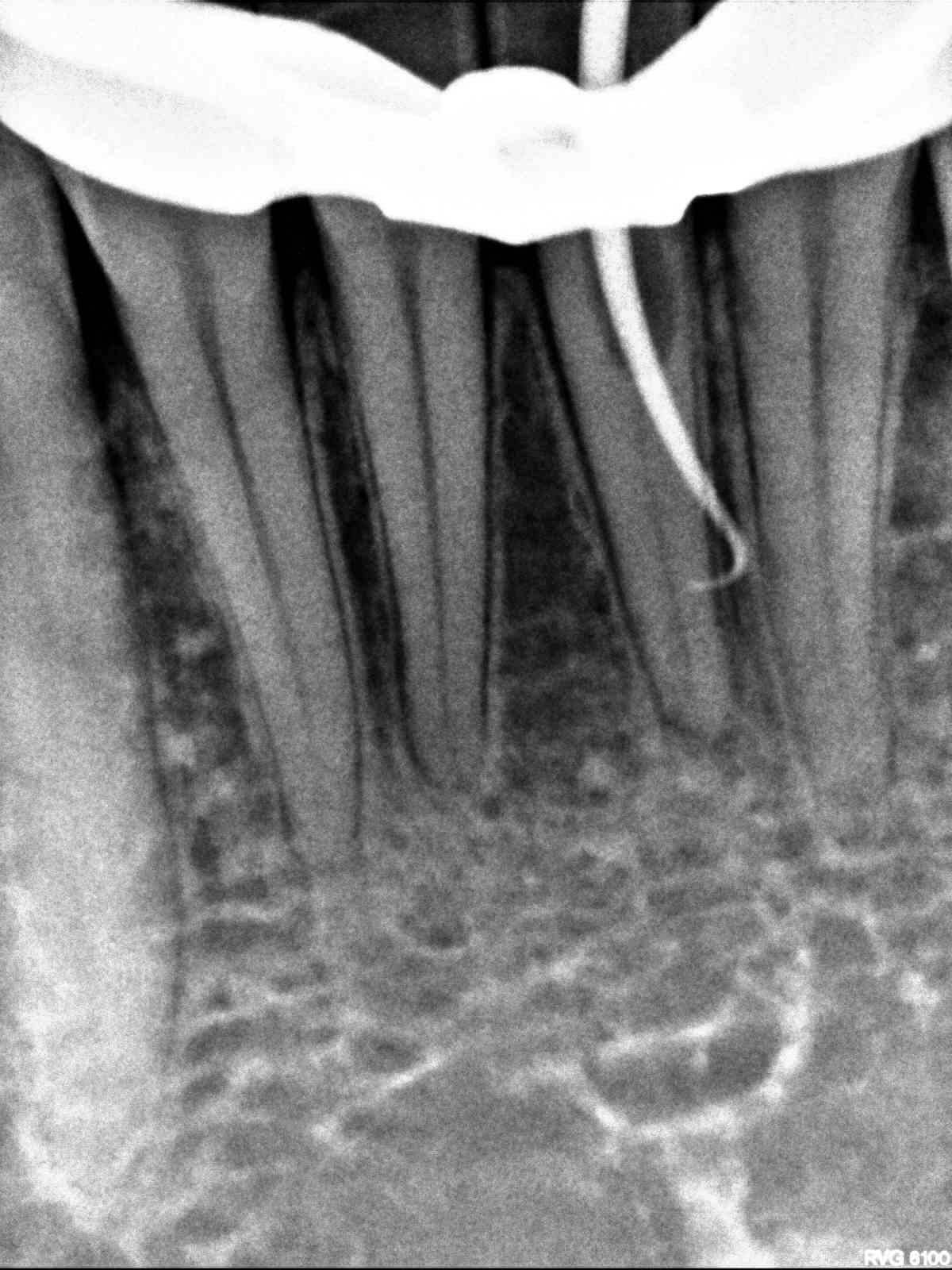
The perforation site was sealed with MTA and the lingual access was closed with flowable composite. The patient was seen three weeks later at which time the entire soft tissue area had healed normally and there was no evidence of a problem. Both the patient and the referral were very glad that the case had worked out so well and that the patient was asymptomatic.
If cosmetic improvement was desired, I recommended that only external bleaching procedures be performed on this tooth, perhaps with a single tooth bleaching tray . I told the patient that results could be unpredictable but at this point, considering all the complications that had occurred during the initial attempts to treat the tooth endodontically , the patient was more inclined to leave the tooth as is.
This is an excellent example of the importance of working length control and the need to monitor Endo access in three dimensions with cone beam tomography. Labial perforation of such teeth is common where severe calcification is present and it is essential that you are able to monitor your 3 dimensional progress into the tooth before such procedural accidents occur.
Furthermore if your working length (as measured by the apex locator) is not coincidental with the approximate root length, STOP the procedure immediately. Under no circumstances should you continue to use irrigants such as sodium hypochlorite in the suspect area until you are confident you are in the canal. In this case, the Dentist was fortunate that the patient was young and the tissues healed quite nicely.