Does This Cracked Tooth Need Endo?
This Case of the Month features a problem that is becoming more common every day – Cracked Tooth Syndrome. Many cases are referred to me because the referring dentist suspects that the tooth has a crack but is not sure whether endodontic treatment is indicated. This could be because they are not sure how deep the crack is and whether it involves the pulp. Or, in some cases, once the cracked portion of the tooth is removed, the remaining tooth structure is insufficiently strong to retain the restoration. In that situation, elective endodontics is required, NOT because of the actual damage caused by the fracture ( the pulp is normal) but because a post space is required to properly retain a core restoration and eventual full cuspal coverage.

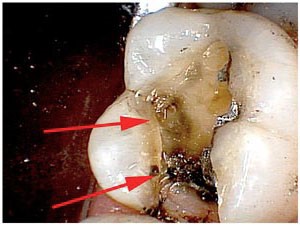

The first test involved application of biting forces to a standard cotton roll. As we advanced from tooth to tooth, we asked the patient to chew on the roll once and then release. When we got to this molar, sensitivity occurred upon release, again another classic sign. Having identified the tooth , we now tried to identify which portions of the tooth were weak. A Tooth Slooth was applied to each cusp individually until we found that the Mesio-Lingual cusp yielded a positive sharp response. We had our culprit. But the question remained…how do we deal with this? Exactly how “Cracked” was the tooth? How far did the crack go? Did it need endodontic treatment? We would need to remove the restoration to find out more.
Application of a small amount of force to the cusp with the back of a mirror handle resulted in a break at the level just below the gingival crest. ( Although removing weak portion of teeth by causing “intentional” cusp fractures such as this seems drastic. It is certainly better than attempting to salvage the cusp, only to have it break later at a far more subgingival level. That can sometimes result in the need for crown lengthening procedures or extraction if the break is too far apical to be treated.)
We obtained a nice clean surface with no signs of pulpal involvement.

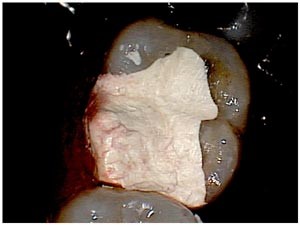
Having determined that the pulp was not involved, we now moved to the stage where we evaluate whether elective endodontics is required. This molar appeared to have good support for the remaining cusps. No other evidence of fractures was visible and the tooth was not in particularly heavy occlusion. I decided that elective endodontic treatment was not required and the case was restored interim with a dressing of IRM.
The patient was asked to monitor the area for a few weeks to confirm symptoms were gone. Correspondence ( including these pictures) was sent to the referral explaining my findings .
It was then up to the restoring Dentist to determine how best to restore the tooth (onlay? Crown?). It is possible that we may have saved the tooth from having further Endodontic treatment, but that will depend on the integrity of the rest of the tooth, the restoring Dentist’s treatment plan and the pulpal response to further restoration.
