Treatment Planning a Fractured Cuspid
A 43-year-old male in good health was referred to my office for examination of tooth #33 (mandibular left cuspid) . This virgin tooth had been involved in a trauma and was now symptomatic to chewing and thermal stimulus. The case had been referred to me for endodontic treatment, but several other questions needed to be answered before we could determine whether endodontic treatment was warranted.
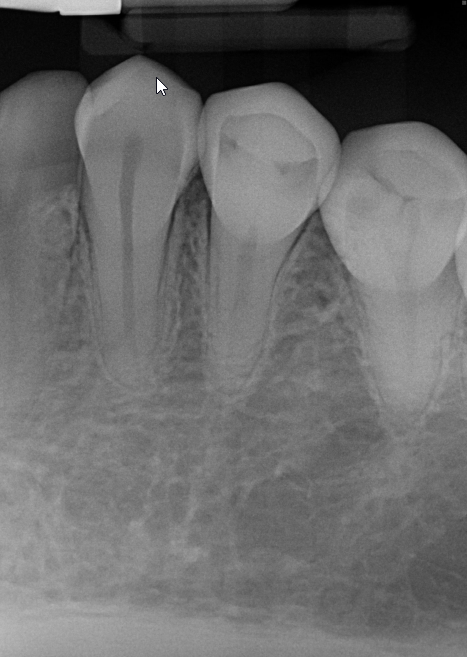
Figure1: Referring Dentist Prop Image
Image of #33 (Mandibular left cuspid) foreshortened but shows no unusual periapical radiolucent findings.
Examination of the Tooth showed a horizontal fracture running along the buccal crown face. Placing buccal pressure on the cusp tip allow the fractured incisal portion to move and the crack opened slightly.

Figure 3: Transillumination of the fracture
Transillumination confirmed that this area was cracked and that this piece was loose.
Figure 3: Transillumination of the fracture
Transillumination confirmed that this area was cracked and that this piece was loose.


Figure 4: Another view of fracture
Placing labial pressure on the cusp tip caused the crack to open and become more visible.
The extent of Fractures of the anterior dentition are often related to the energy that is transferred to the tooth during trauma. Living a cold winter climate means that I see a lot of hockey related injuries (pucks and sticks) as well as slips and falls on ice due to loss of footing.
Fractures generally fall under two categories:
1. Fractures in which the incisal edge is sheared off horizontally in a “clean break”. Generally, this is from a puck, baseball, projectile hitting the object at high speed with limited mass. Forces (Kinetic energy KE= 1/2 MV(squared)) are concentrated and the tooth often (but not always) shears off cleanly near the site of impact. In those cases, the pulp may or may not be exposed by the broken part of the tooth. The cleanly fractured piece can often be rebonded to the tooth ( after endo, if necessary) and the integrity and aesthetics of the tooth is fully restored without the need for further treatment if there is no pulp exposure.
2. Compound fractures These fractures often occur with large mass objects or falls in with very large forces are applied to the tooth that results in compound fractures of the tooth/root. ( Cross checking by hockey stick, slip and fall on ice or off of a bike) The tooth essentially “shatters”. Most often the fracture line on the buccal aspect ( from which the forces are applied) causes oblique fractures that are either crestal or subcrestal on the palatal/lingual aspect. The ability to restore these teeth depends on the extent of the fracture in this area and whether it can be managed periodontally and restoratively.
Several questions need to be addressed as we treatment plan the case:
1. How deep is the fracture and have ALL the fractured portions of the tooth been removed to examine the extent of tooth loss?
- Can the tooth be restored with a margin that is not too far subgingival that it results in a chronic postop periodontal problem? Is crown lengthening indicated if the fractured portion can not be rebonded? Would forced eruption ( to eventually expose a manageable lingual margin) be a better option that crown lengthening? (This depends on the particular situation i.e./ root length, periodontal support, tooth position.)
- Would extraction and replacement with an implant be a better option than trying to save the tooth?
I consulted with the Periodontist involved with the case and explained that we could NOT initiate Endodontic treatment until a comprehensive treatment plan was formulated and presented to the patient. The patient was eager to save the tooth but I believed that we needed to explain that we didn’t know enough about the fracture at the moment to determine whether this was feasible.
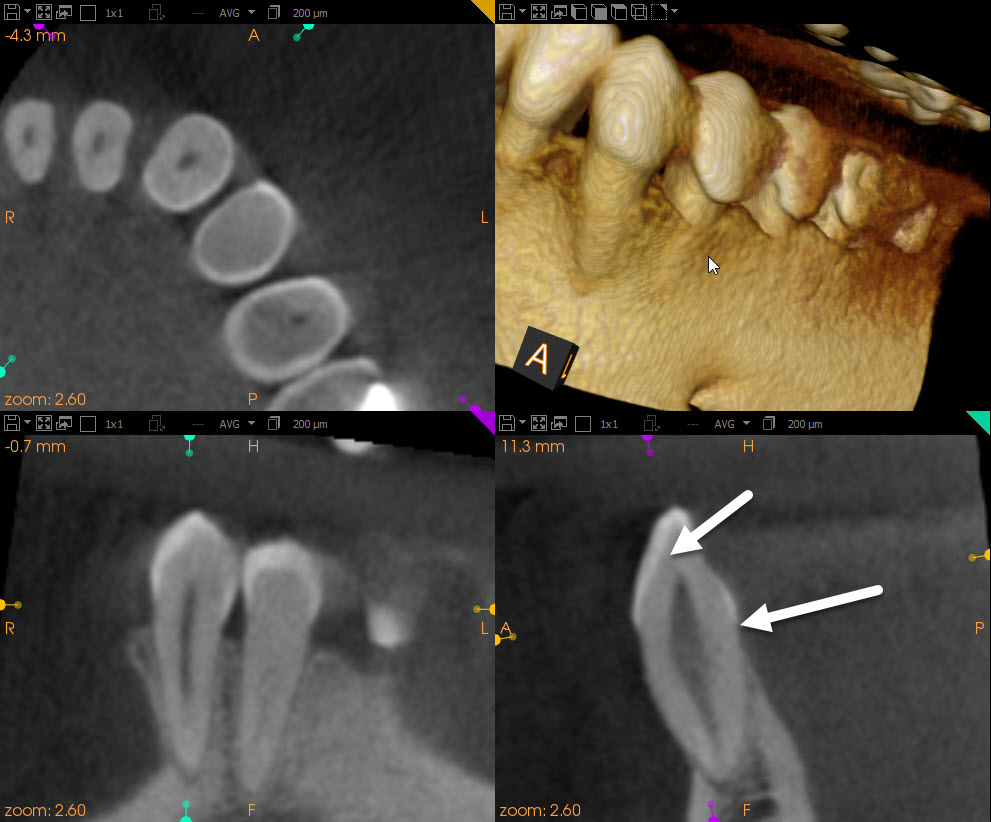
The cbCT image showed a very faint radiolucent line that seemed to suggest the extent of the fracture was limited to the area between the two arrows in the above cbCT slice. If so, the prognosis was much better. However, the fractured portion of the tooth would still need to be removed to confirm this prognosis.
In the cbCT, we also noted that the cuspid root length was atypically short and that there was literally no bone covering the buccal aspect of the root. Extraction of the tooth and attempted implant placement would be difficult and invariably result in the need for significant bone grafting to allow for proper placement of the implant inside bone. So, from the looks of the cbCT, the implant option was not practical.
I concluded that Endodontic treatment of this cuspid was not the issue.
The real concerns are:
1. Where is the lingual extent of the fracture?
2. Is the fracture compound in nature?
3. Can a manageable, Periodontally healthy crown margin be obtained with some kind of Perio surgery or Ortho extrusion intervention?
I told the Periodontist that until these questions were answered, it made little sense to consider Endodontic treatment. I suggested a combined approach where the Periodontist would remove the fractured portion, determine restorability ( in consultation with the restoring dentist) and then send the patient to me once a treatment plan and strategy had been confirmed. If suitable or possible, the fractured portion could be retained and rebonded after the Endo treatment had been completed. If they determined that the fracture had rendered the tooth unrestorable, other strategies for replacement (bridge?) may have to be considered and endo would not be necessary.
Although patients are frequently referred to an Endodontist for “a procedure”, it is incumbent on Specialists and referring Dentists to recognize other problems and concerns and to make sure they are addressed in the overall treatment plan.