BWs and Communication with the Referral Best Manages the Case
A 52 year old male patient was referred for Endodontic treatment of a mandibular left first molar. The patient had a history of gross swelling in the buccal vestibule adjacent to the tooth. The tooth had been restored with full gold Crown and the referring dentist saw a periapical radiolucent finding at the apices, diagnosed an acute apical abscess and requested that I perform Endodontic treatment through the Crown. The patient was given an antibiotic and by the time he arrived in my office, he was relatively asymptomatic aside from some chewing and buccal palpation sensitivity.


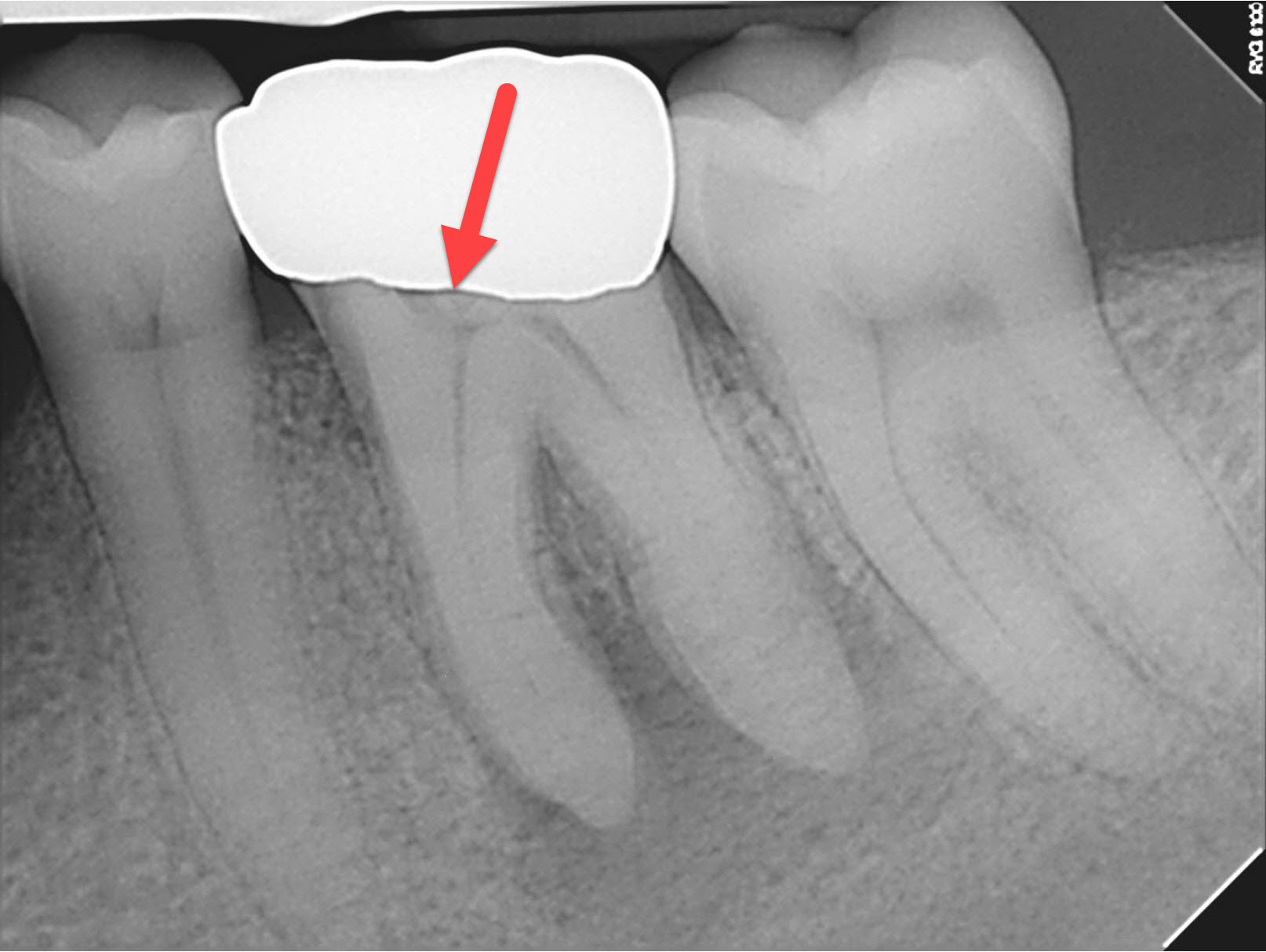
It is customary for my staff to take a new periapical image and a bitewing radiograph for any posterior tooth that we are considering treating. The referral’s periapical image did not show anything unusual, but my periapical image and the bitewing showed a radiolucent finding underneath the mesial aspect of the Crown margin (red arrow below). The bite wing clearly showed the defect was significant. It was close to the bone crest. Was that ECIR? (External resorption?) Closer examination of the mesio-buccal Crown margin showed what appeared to be an abfraction lesion or possible carries in this area. The clinical appearance was quite unusual because the area did not feel like caries or an ECIR when explored. The surface of the defect felt smooth but I was pretty sure that this was not a short margin. The defect was deep enough that I thought it may be close to communicating with the pulp. Whatever it was, it needed to be examined and dealt with before the endodontics could be started.
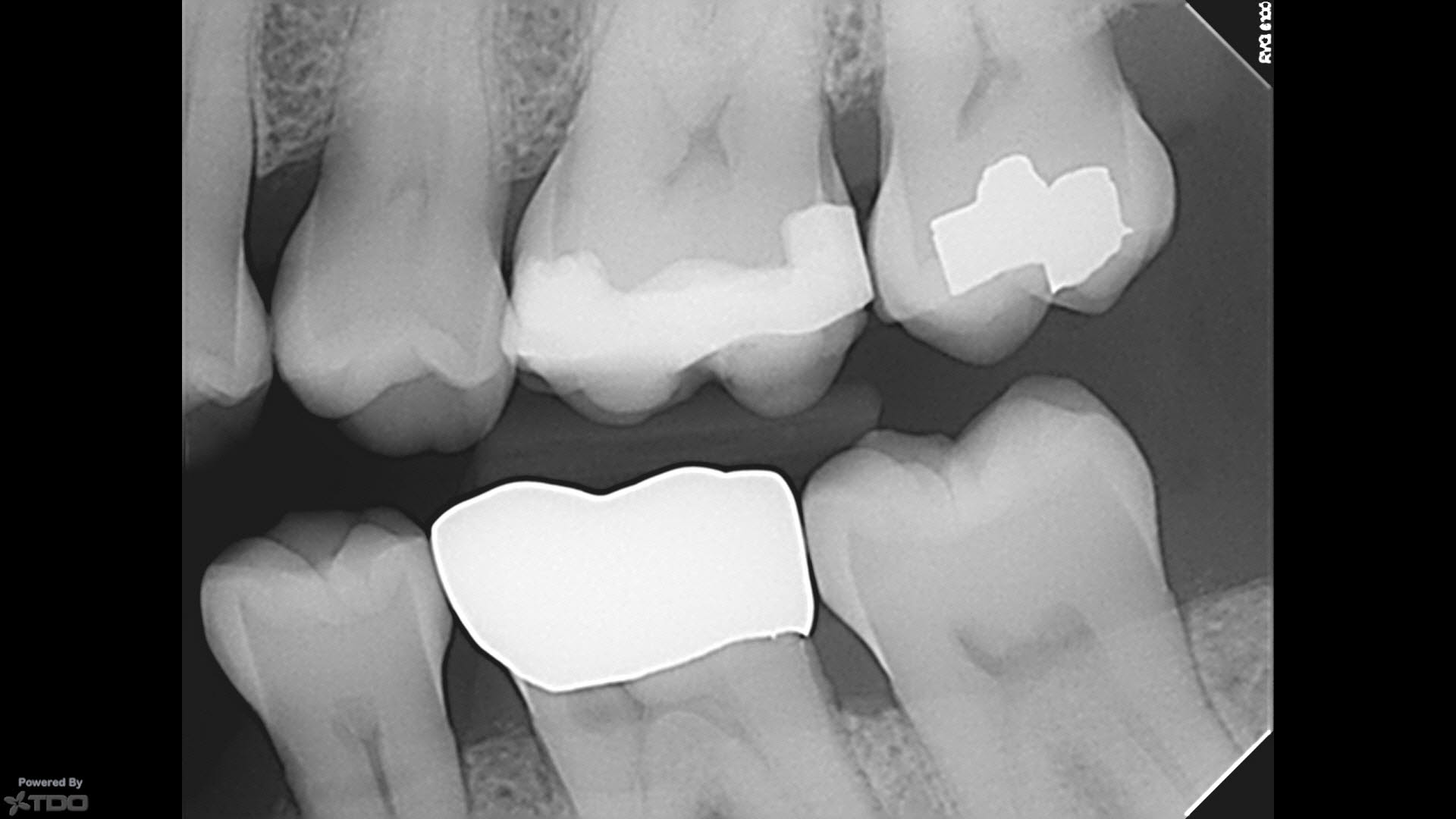
In any case, this problem would need to be assessed during treatment planning of this tooth. Further pre-treatment (removal of the crown at a minimum) and exploration of the defect would need to be performed. Crown lengthening may be necessary which may place the whole re-restoration aspect of the new Crown in jeopardy because of the proximity to the furca. Certainly the patient would want to know if further Periodontal procedures would be required prior to us attempting to restore the tooth. Ultimately, we do not want to create a situation where chronic Periodontal problems make management of this buccal margin difficult for the patient, leading to hygiene issues, further caries or eventual extraction.
If we added the costs of Crown lengthening to the Endodontic treatment and new Crown, we are starting to get close to the cost of extraction and replacement with an implant.
I contacted the referring dentist and told them that there was a defect on the mesial aspect of the tooth. I could not in good conscience continue to perform the Endodontic treatment until the Crown was removed and the referring dentist assessed the tooth for restorability in his office. If further procedures were necessary, he would have to decide whether the Crown margin was at an acceptable level and whether further Periodontal procedures would be necessary. All these procedures and the associated costs would have to be explained to the patient before we initiated Endodontic treatment and committed the patient to rehabilitation of the tooth.
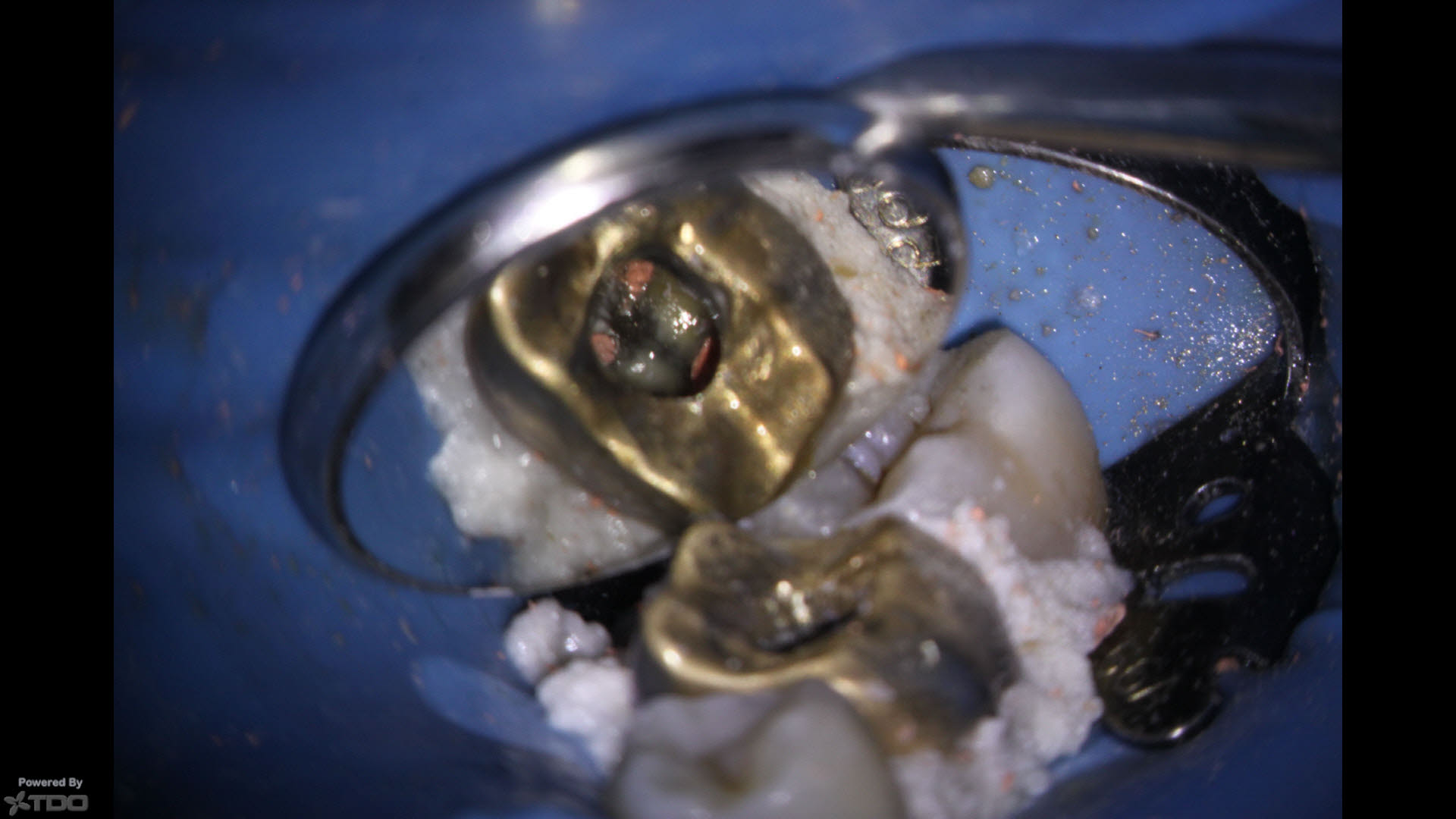
The patient returned to his dentist and I subsequently received this note: “The gold crown was removed with crown removing forceps The amalgam core is intact with good tooth ferrule. Margins were re-prepped deeper along the buccal. The crown was re-luted with Voco Bifix temp cement, with the open margin on the buccal sealed. I believe I can restore the tooth in its current condition. Please proceed with the Endodontics.”
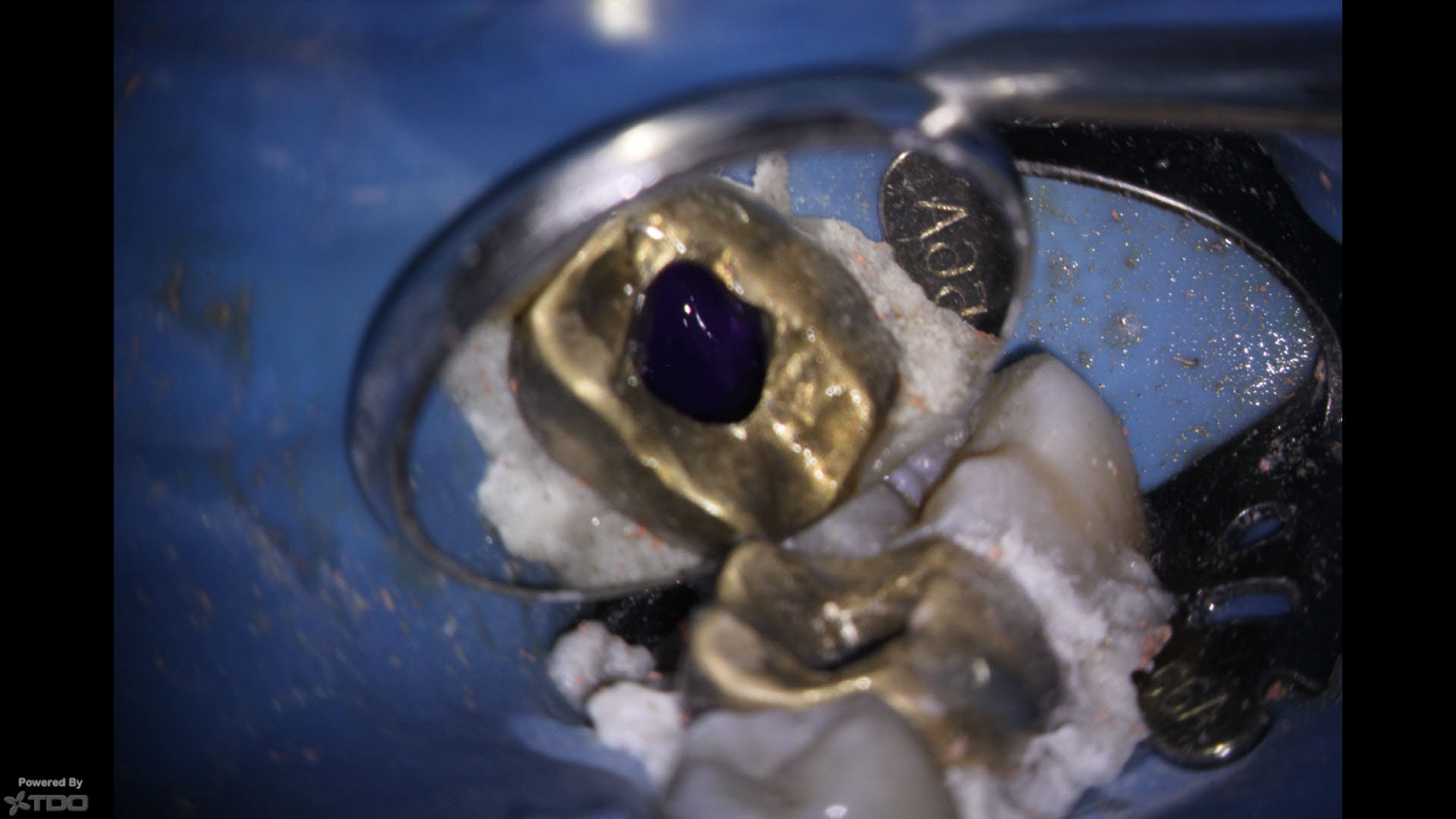
Since the crown seemed secure and was going to be remade, I chose to access through it. The case was cleaned and shaped and medicated with Ca(OH)2. The patient returned several weeks later, asymptomatic, at which time we obturated the case. The crown was sufficiently sealed that I was confident the defective area would not be an issue between appointments and the tooth was ultimately restored.
Coordination of the treatment and good communication with the referring Dentist allowed us to achieve the optimal results with no compromises.
In any case, this problem would need to be assessed during treatment planning of this tooth. Further pre-treatment (removal of the crown at a minimum) and exploration of the defect would need to be performed. Crown lengthening may be necessary which may place the whole re-restoration aspect of the new Crown in jeopardy because of the proximity to the furca. Certainly the patient would want to know if further Periodontal procedures would be required prior to us attempting to restore the tooth. Ultimately, we do not want to create a situation where chronic Periodontal problems make management of this buccal margin difficult for the patient, leading to further gingival problems, further caries or eventual extraction.
If we added the costs of Crown lengthening to the Endodontic treatment and new Crown, we are starting to get close to the cost of extraction and replacement with an implant.
I contacted the referring dentist and told them that there was a defect on the mesial aspect of the tooth. I could not in good conscience continue to perform the Endodontic treatment until the Crown was removed and the referring dentist assessed the tooth for restorability in his office. If further procedures were necessary, he would have to decide whether the Crown margin was at an acceptable level and whether further Periodontal procedures would be necessary. All these procedures and the associated costs would have to be explained to the patient before we initiated Endodontic treatment and committed the patient to rehabilitation of the tooth.
The patient returned to his dentist and I subsequently received this note: “The gold crown was removed with crown removing forceps The amalgam core is intact with good tooth ferrule. Margins were re-prepped deeper along the buccal. The crown was reluted with Voco Bifix temp cement, with the open margin on the buccal sealed. I believe I can restore the tooth in its current condition. Please proceed with the Endodontics.”
Since the crown seemed secure and was going to be remade, I chose to access through it. The case was cleaned and shaped and medicated with Ca(OH)2. The patient returned several weeks later, asymptomatic, at which time we obturated the case. The crown was sufficiently sealed that I was confident the defective area would not be an issue between appointments and the tooth was ultimately restored.


Coordination of the treatment and good communication with the referring Dentist allowed us to achieve the optimal results with no compromises.



A 6 month recall the pocketing had resolved, the furcal bone appeared to be filling in and the periapical radiolucency appeared to be resolving. The patient was asymptomatic.
However, much t my dismay, there appeared to be a void under the crown margin ( in the chamber?) that may indicate that the temporary sponges were never removed or that this area remained unfilled. Although an orifice bond was performed by me after the Endo, any open space in the chamber has the potential for coronal leakage that may contribute to long term Endo failure.
