Treatment Plan or Fail ?
For today’s case of the month we discuss treatment planning with regards to this important maxillary first molar distal abutment. The patient presented with evidence of curious involvement of the distal aspect of tooth #26. The contact between #26 and 27 was open resulting in deep distal decay underneath the Crown margin of #26. The referring Dentist took a novel approach of simply cutting a DO preparation into this distal abutment crown, excavating the decay and temporizing it with IRM.
If we simply look at the periapical image, we see that the contact is open and that the open contact has likely resulted in continued problems with maintaining hygiene on the distal aspect of this important abutment tooth. #26 is part of a four unit bridge that is integral to the patients function on this site. The abutments for this bridge are #25 and 26 with a unique onlay/rest on the palatal aspect of #23. The anterior portion of the bridge is cantilevered onto this cuspid, which may have contributed to the lifting and/or opening of the Distal margin of the #26 crown abutment.

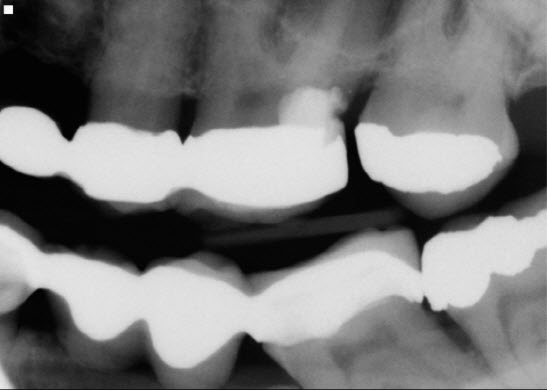
Examination of the bitewing radiograph gives us more information and a clue as to why this problem persists. The restoring dentist had placed an opposing mandibular bridge using tooth #36 as a very tilted distal abutment. Because the distal marginal ridge of #36 was above the occlusal plane, it acted as a plunger cusp forcing open the contact between the two maxillary molars. This situation was destined to create continued problems with food impaction in the maxilla. Unless we addressed this issue, endodontic treatment of #26 and attempted repair of the distal margin or replacement of the MO amalgam in #28 to try to close the contact, would likely fail. This did also not address the cantilever tipping forces on the mesial aspect of the bridge in the area of #s 23 and 24. The whole side was a disaster.



So we were faced with a difficult decision of how to deal with this. One of the ways we could solve problem was to simply remove the maxillary second molar. Endodontic treatment could be performed on the maxillary first molar and an attempt could be made to repair the distal margin of the maxillary first molar if the patient was not interested in replacing the entire bridge. This was , at best, a stopgap measure, destined to ultimately fail. The patient would lose some posterior function due to the extraction of #27 (leaving #37 unopposed,) but this is the price we would pay to ensure that the maxillary bridge could be maintained with proper hygiene. Unfortunately, this would still leave unfavorable occlusal forces on the bridge and eventual loss of the bridge. But it may provide a short term affordable option for the patient. Endo would therefore be necessary of #26 and treatment would need to be scheduled.
Ideally, the bridge should be replaced but this is not always financially feasible. We could also extract #26, and create a new bridge with abutments #23-25 and 27. Again, the rocky occlusal plane in the mandible may make this impossible. For proper restoration, establishment of a more even occlusal plane would be necessary, which would likely involve re-restoration of that side of the mandible, unaffordable for the patient at the time.
So whose responsibility is it to go over these strategies and possible treatment plans with the patient? And if the patient is just referred for endodontic treatment of #26, is it within the prerogative of the Endodontist to discuss this with the patient ?
Long term endodontic success can only be achieved when the coronal seal is maintained. If we simply Endodontically treat the maxillary molar as requested , I have no doubt that decay will recur and that the long term success of the endodontics may be compromised.
