Are You SURE its Endo?


Add a Title
This patient was seen for endodontic consideration of #16. The tooth had been restored with a composite. The tooth had a crack that ran from the mesial marginal ridge distally through the composite., The patient was complaining of Percussion, Biting and Chewing sensitivity. Cold tests were non responsive. This tooth was opposed by a full crown. (As MANY cracked teeth often ARE!)
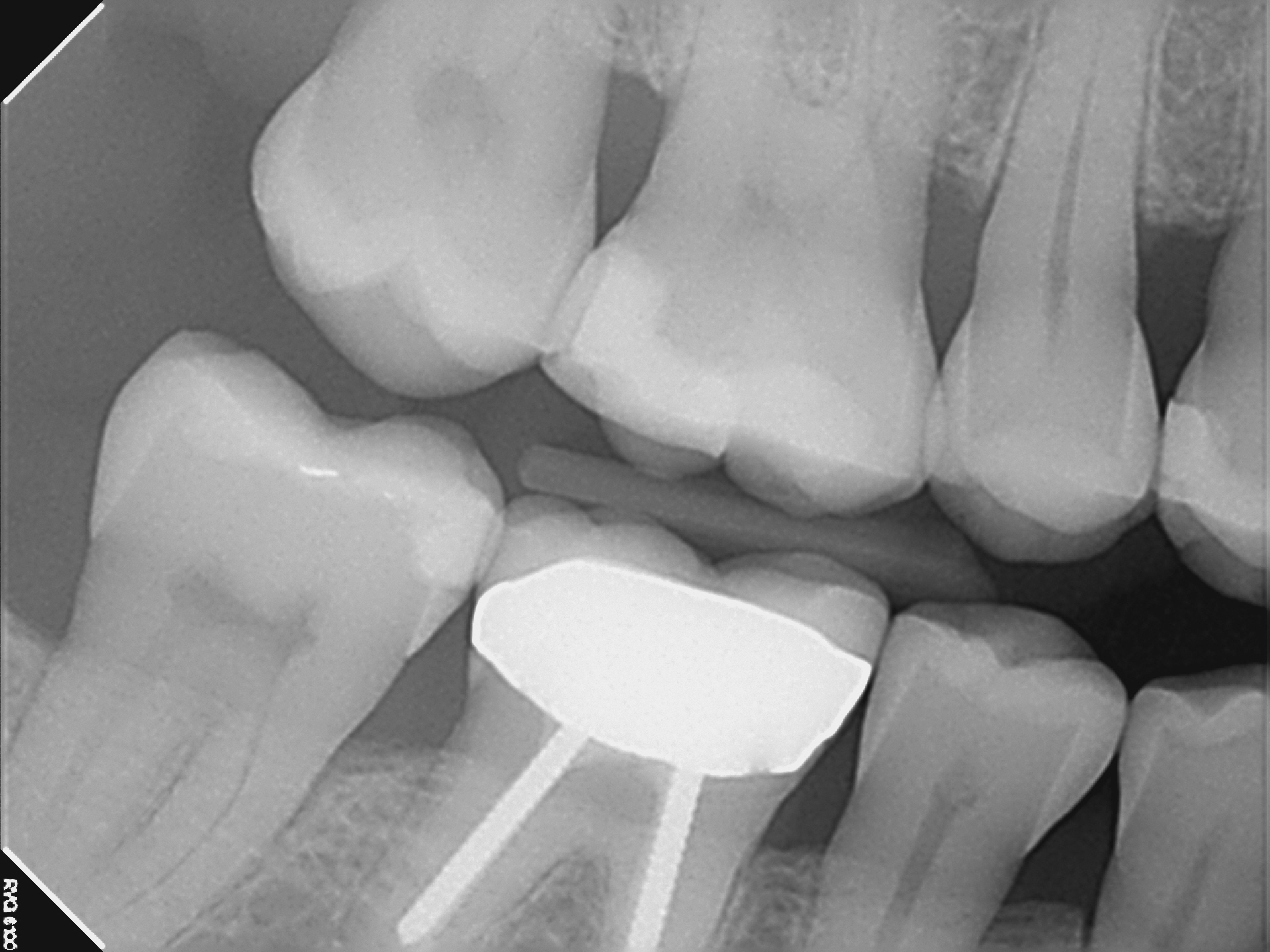
Radiography revealed a shallow/moderate depth DO composite with no evidence of possible pulp exposure or other unusual radiolucent periapical findings consistent with pulpal necrosis. I noted some horizontal bone loss on the bite wing. Probings were WNL.
A diagnosis of pulpal necrosis was made (possibly due to the crack) with normal periapex. Conventional endodontic treatment was scheduled. The distal and palatal canals were cleaned and shaped and medicated . The MB canals were extremely calcified at the midroot and required more work during a subsequent appointment. Ultimately, they were not negotiable to the terminus and the clinical radiographic results were less than what I had hoped. However, the patient was asymptomatic after the initial appointment and I decided to obturate the case as best i could. The tooth was promptly restored with a full Crown restoration by the referring Dentist.



Approximately a year later, the referral called my office saying that the patient was having symptoms in the area and asked that I see the patient for follow up.
Examination of the crowned tooth revealed normal responses to chewing, percussion and palpation. Periapical areas appeared to be within normal limits on the radiograph and there was no sign of pathology associated with the previously short filled mesial buccal root.
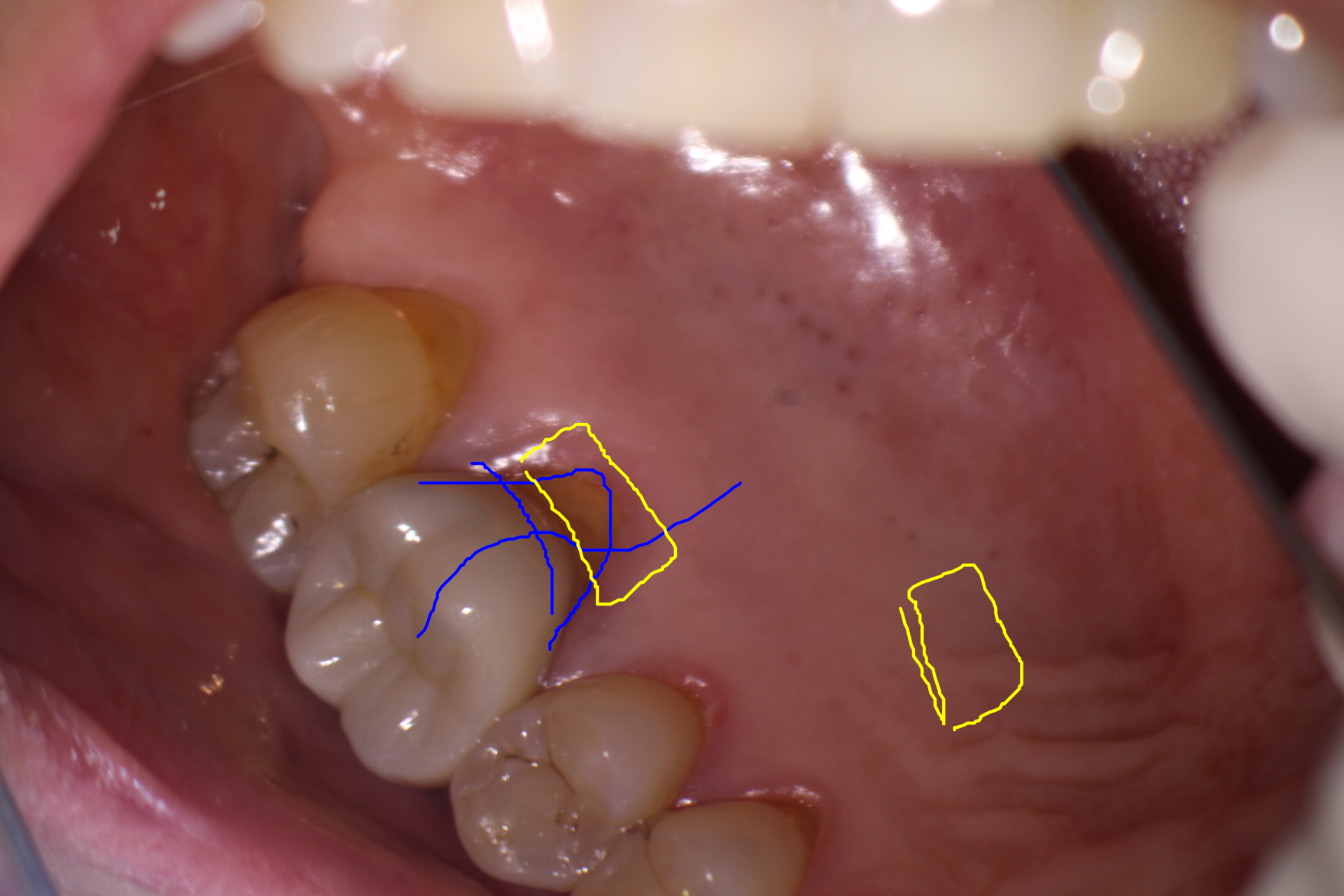
The patient remarked that the symptoms appeared to be more centered on the palatal gingiva, at which time I noticed that there had been increased recession of the gingiva in that area since initial Endo treatment had been performed in my office.
Probing the palatal gingival pockets with a Perio probe elicited the exact patient current complaint. The gingival crest tissue appeared to be slightly red and tender and the patient remarked that this was the pain that she was getting when she was eating.

I suggested that this could be handled either of two ways:
(1) Referral to a Periodontist to see if a free gingival graft was a possibility to cover the exposed root (?) OR
(2) Remove the existing Crown and re-prepare the Crown margin slightly lower to encompass this receded area, while at the same time adjusting the palatal contour of the Crown for comfort. Once a temporary Crown had been placed with a comfortable contour that deflected food away from the symptomatic area, the Dentist could leave this in for several months to see if the gingiva stabilizes and the symptoms resolve. If so, a new permanent Crown would be cemented to match the existing contours of the asymptomatic temporary crown.
In any case, it was clear that Endodontic retreatment was not required.
It is not uncommon for Endodontists to have patients return to their office for issues that are entirely unrelated to the previous treatment. Although Endodontists limit the practice to Endodontics, it is natural that (because we are frequently called upon to diagnose oral pain), we must know and recognize problems in all other areas of dentistry whether they be periodontal, occlusal, TMD, Orofacial, Prosthetic or Endodontic in etiology.
There is a tendency for Dentists to look at a symptomatic patient’s image on radiograph, detect an Endodontic treatment and assume the problem to be Endo related, and immediately refer the case to the Endodontist. Before you consider doing this on a previously Endo treated case, make sure to listen to the patient’s current complaint closely and you frequently will find that while the tooth may have been Endodontically treated, the patient’s current complaint has little to do with previous Endodontics.
