Treatment Planning a Trauma Case
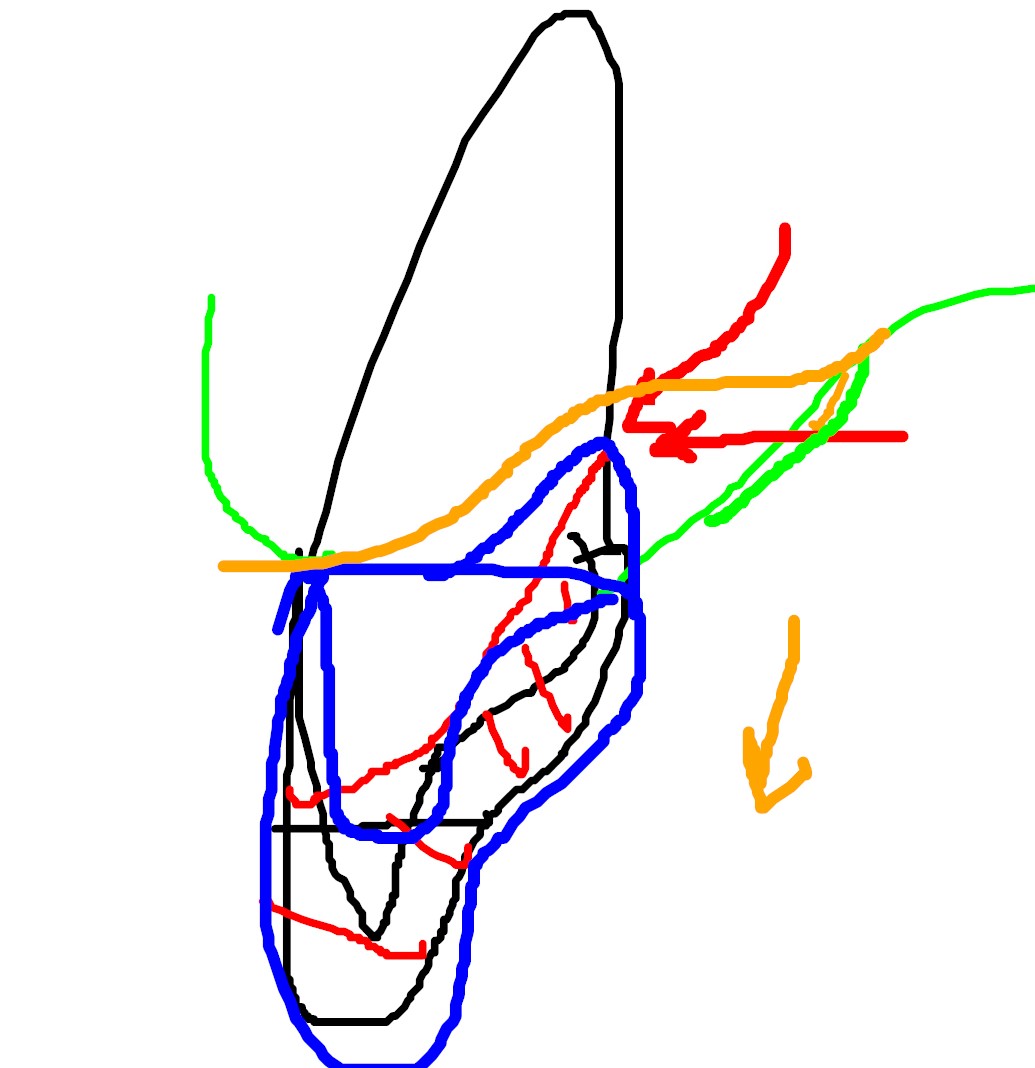
This 23 year old patient was seen for examination regarding tooth #11 -the maxillary central incisor. The patient had a significant history of taking a high stick to the face during a hockey game . The coronal aspect of #11 was fractured (Ellis class 3 MID) during the accident. I noted a 5 millimeter probing in the area of the palatal fracture and associated draining buccal sinus. The oblique fracture is typical in that the buccal portion cracks in the mid root while the palatal extent is far subgingival – at the bone Crest. A diagnosis of chronic periodical periodontitis secondary to pulpal necrosis was made . The other maxillary and mandibular teeth tested normally to pulp tests. No other endodontic treatment was required. The patient was lucky, the accident could have resulted in more severe injury.
The determining factor as to whether we wish to restore this tooth is based more upon restorative and other factors rather than endodontic factors. There are three factors that must be assessed before we decide whether to initiate Endodontic treatment and start the patient on the journey to rehabilitate the tooth.
#1. – The extent of the fracture on the palatal side
There is no question that the tooth cannot be restored as it presented. We will need to either extract it and replace it prosthetically or attempt to somehow obtain access to the fracture area to allow the restoring dentist to place an adequate palatal Crown margin after the Endo has been completed
#2 – The maxillary arch crowding
The anterior maxilla exhibits generalized tooth size/arch size discrepancy. This has resulted in rotation of the centrals about 40 degrees, which makes re-restoration of #11 challenging. In order to even out the centrals in terms of mesial distal width, the restoring dentist would probably have to slice or veneer the virgin #21. Either way, the restored centrals will have reduced mesial-distal width and less than optimal aesthetics.
The ideal scenario would be to place maxillary full arch orthodontics, optimally align the centrals and the rotated cuspid #23,. Ortho hardware would also allow us to perform forced eruption of #11 after endodontics is completed in order to expose the palatal Crown margin. The maxillary anteriors could then be position for optimal restoration of #11. to match the virgin #21. This is a far more extensive treatment plan but it would give us the optimal result.
I obtained a consult from a periodontist in my building about the possibility of Perio Crown lengthening. She said that she would like to try to avoid any attempted Crown lengthening procedures on the palatal aspect of #11 because of the amount of hard and soft tissue loss that would need to take place to properly Crown lengthen the tooth. Furthermore she said we may compromise the adjacent papilla should we get recession after the surgery . In THAT case, Endo treatment would be CONTRAINDICATED.
#3 – Extraction and implant replacement
Lastly, we could extract the tooth and place an implant but that still leaves us with the crowding issue.
By the time we pay for the implant we probably could have had Orthodontic treatment/forced eruption and restore #11 optimally after the Endo.
I suggested that the referring dentist create some study models and consult with an Orthodontist to see how to restore this tooth in a manner that is acceptable to the patient in the way of aesthetics, time, and cost.




Treatment Planning a Trauma Case
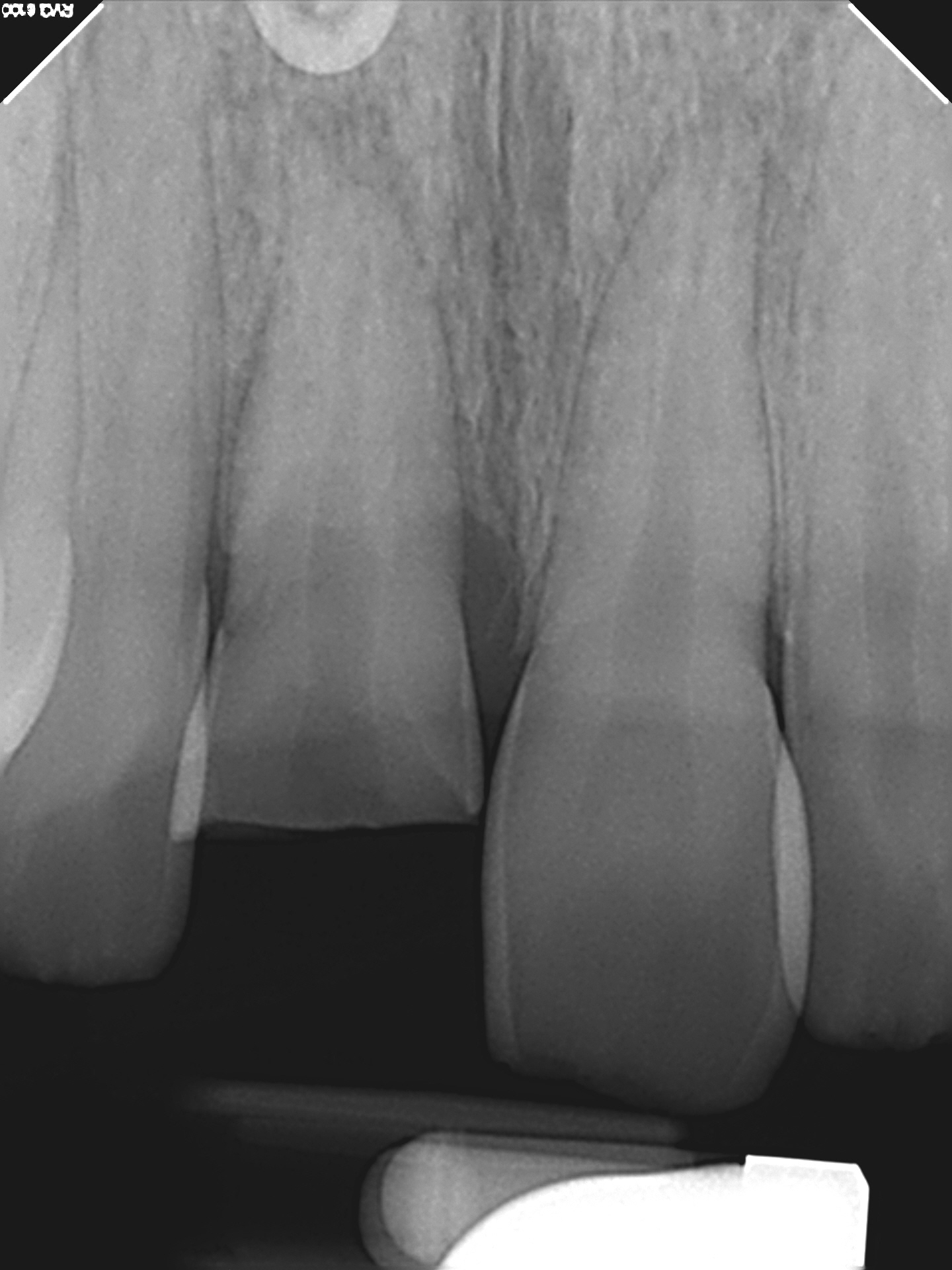
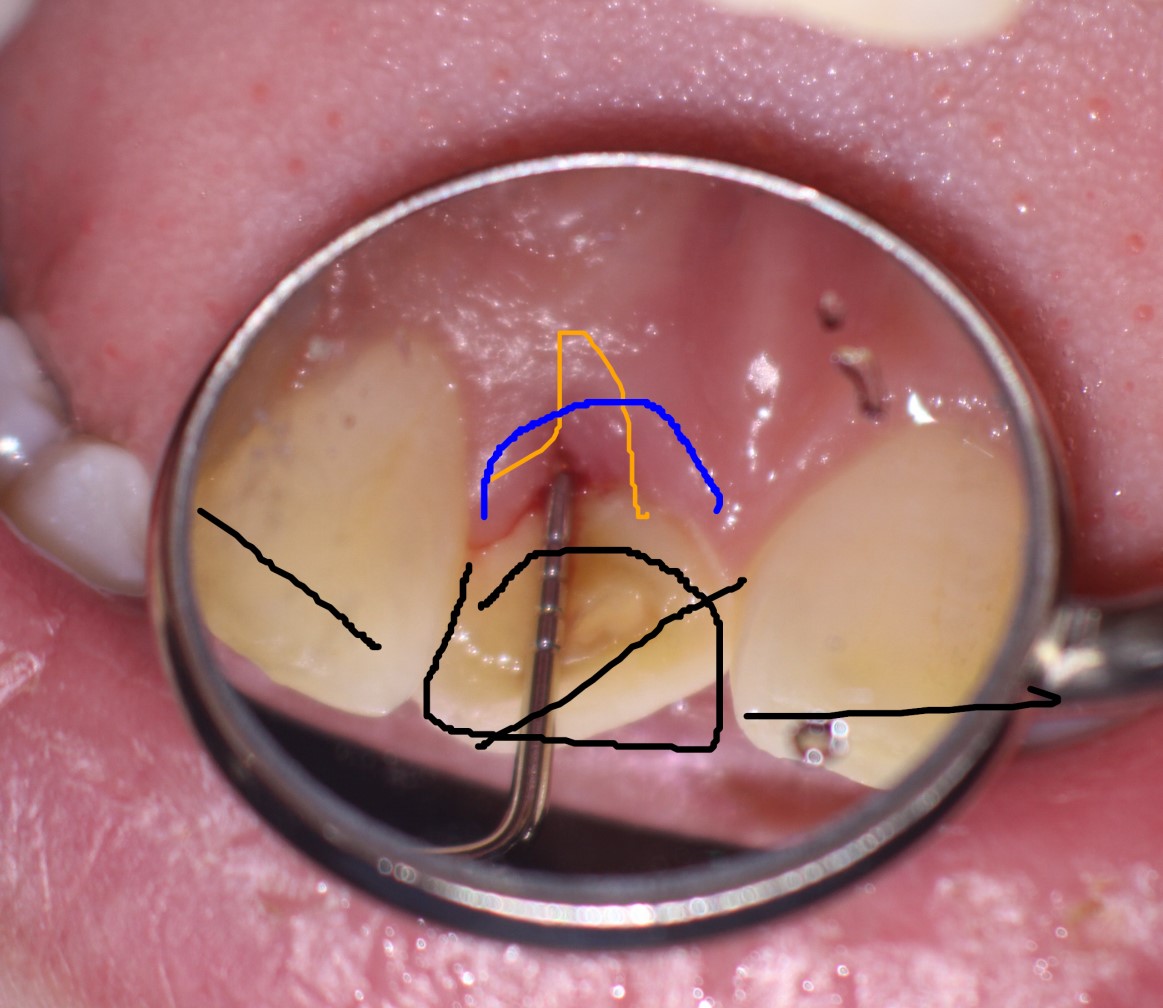
This 23 year old patient was seen for examination regarding tooth #11 -the maxillary central incisor. The patient had a significant history of taking a high stick to the face during a hockey game . The coronal aspect of #11 was fractured (Ellis class 3 MID) during the accident. I noted a 5 millimeter probing in the area of the palatal fracture and associated draining buccal sinus. The oblique fracture is typical in that the buccal portion cracks in the mid root while the palatal extent is far subgingival – at the bone Crest. I also noted some significant horizontal bone loss associated with #11. This would prove to be an important observation later in the treatment planning. A diagnosis of chronic periodical periodontitis secondary to pulpal necrosis was made . #31 had an MID incisal chip from the injury as well. But all the other maxillary and mandibular teeth (aside from #11) tested normally to pulp tests. No other endodontic treatment was required. The patient was lucky, the accident could have resulted in a much more severe injury.
We needed to determine whether we wished to initiate Endodontic treatment and embark on the protracted sequence of treatment that would be needed to rehabilitate the tooth. That decision was based far more upon restorative and other factors rather than endodontic factors.
I felt that there were three factors that had to be assessed by all the clinicians involved in the rehabilitation:
#1. – The extent of the fracture on the palatal side
There is no question that the tooth could be restored as it presented. We will need to either extract it and replace it prosthetically or attempt to somehow obtain access to the fracture area to allow the restoring dentist to place an adequate palatal Crown margin after the Endo has been completed
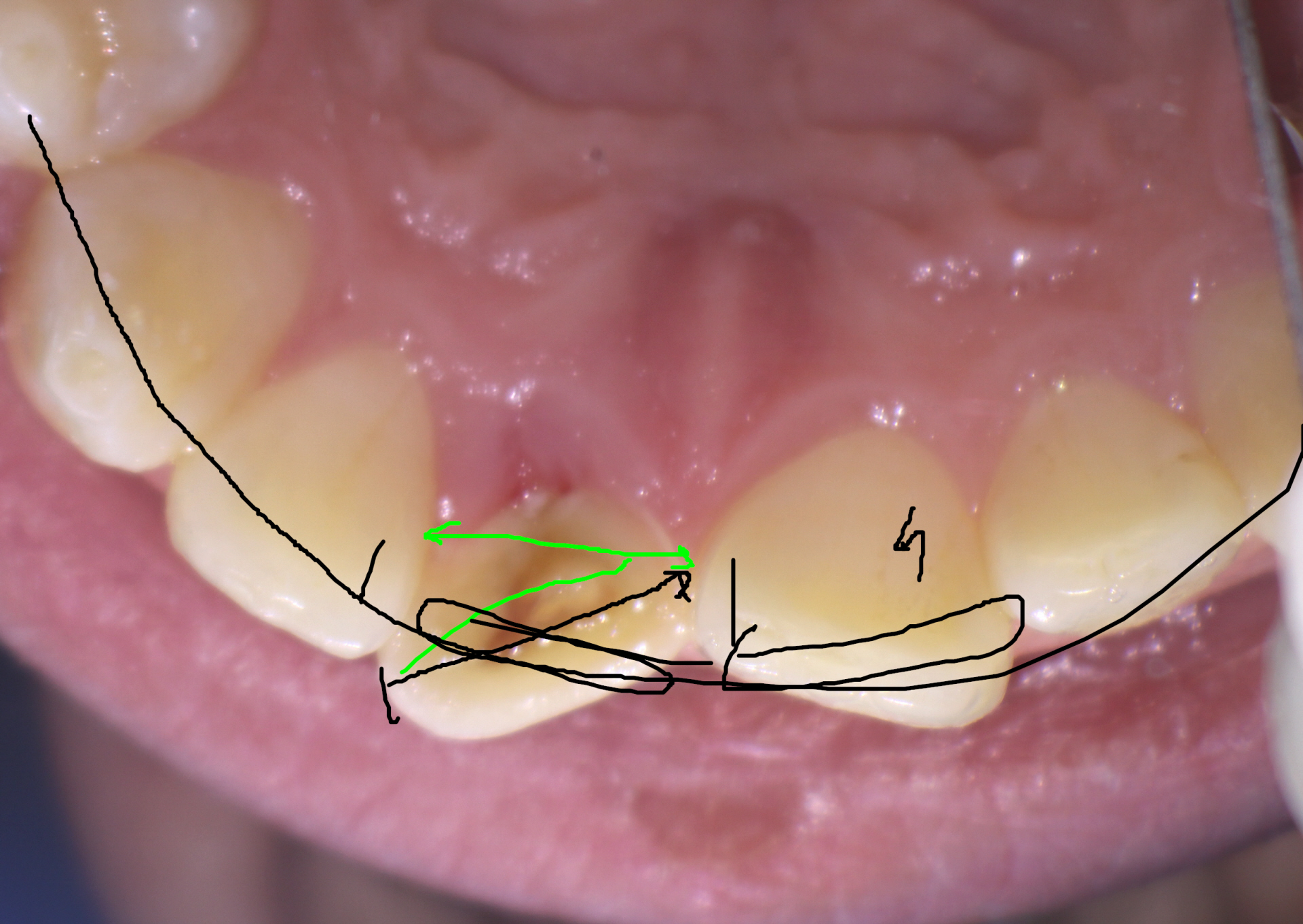
#2 – The maxillary arch crowding
The anterior maxilla exhibits generalized tooth size/arch size discrepancy. This has resulted in rotation of the centrals about 40 degrees, which makes re-restoration of #11 challenging unless we wanted to merely place an implant and recreate the crowded/rotated position of #11 (hardly ideal) . In order to “even out” the centrals in terms of mesial distal width, the restoring dentist would probably have to slice or veneer the virgin #21. Either way, the restored centrals will have reduced mesial-distal width and less than optimal aesthetics unless we dealt with the crowding Orthodontically prior to restoration of either the natural #11 or implant #11.
The ideal scenario would be to place maxillary full arch orthodontics, optimally align the centrals and the rotated cuspid #23,. Ortho hardware MAY also allow us to perform forced eruption of #11 after endodontics is completed in order to expose the palatal Crown margin. (But I the root was not particularly long and I was unsure about the crestal bone loss that already had occurred next to the fracture site. )The maxillary anteriors could then be position for optimal restoration of #11, to match the virgin #21. This is a far more extensive treatment plan but it would give us the optimal result.
I obtained a consult from a periodontist in my building about the possibility of Perio Crown lengthening. She said that she would like to try to avoid any attempted Crown lengthening procedures on the palatal aspect of #11 because of the amount of hard and soft tissue loss that would need to take place to properly Crown lengthen the tooth. Furthermore she said we may compromise the adjacent papilla should we get recession after the surgery . In THAT case, my Endo treatment would be CONTRAINDICATED.
#3 – Extraction and implant replacement
Lastly, we could extract the tooth and place an implant but that still leaves us with the crowding issue and Ortho would likely need to be performed to get teh best results..
The options were many and the choices unclear on presentation. For those reasons, I suggested that the referring dentist create some study models and consult with an Orthodontist to see how to restore this tooth in a manner that is acceptable to the patient in the way of aesthetics, time, and cost. That may. or may not involve Endodontic treatment of the tooth. Simply Endo treating the tooth without these considerations is below the standard of care, in my opinion.
Treatment Planning a Trauma Case
This 23 year old patient was seen for examination regarding tooth #11 -the maxillary central incisor. The patient had a significant history of taking a high stick to the face during a hockey game . The coronal aspect of #11 was fractured (Ellis class 3 MID) during the accident. I noted a 5 millimeter probing in the area of the palatal fracture and associated draining buccal sinus. The oblique fracture is typical in that the buccal portion cracks in the mid root while the palatal extent is far subgingival – at the bone Crest. A diagnosis of chronic periodical periodontitis secondary to pulpal necrosis was made . The other maxillary and mandibular teeth tested normally to pulp tests. No other endodontic treatment was required. The patient was lucky, the accident could have resulted in more severe injury.
The determining factor as to whether we wish to restore this tooth is based more upon restorative and other factors rather than endodontic factors. There are three factors that must be assessed before we decide whether to initiate Endodontic treatment and start the patient on the journey to rehabilitate the tooth.
#1. – The extent of the fracture on the palatal side
There is no question that the tooth cannot be restored as it presented. We will need to either extract it and replace it prosthetically or attempt to somehow obtain access to the fracture area to allow the restoring dentist to place an adequate palatal Crown margin after the Endo has been completed
#2 – The maxillary arch crowding
The anterior maxilla exhibits generalized tooth size/arch size discrepancy. This has resulted in rotation of the centrals about 40 degrees, which makes re-restoration of #11 challenging. In order to even out the centrals in terms of mesial distal width, the restoring dentist would probably have to slice or veneer the virgin #21. Either way, the restored centrals will have reduced mesial-distal width and less than optimal aesthetics.
The ideal scenario would be to place maxillary full arch orthodontics, optimally align the centrals and the rotated cuspid #23,. Ortho hardware would also allow us to perform forced eruption of #11 after endodontics is completed in order to expose the palatal Crown margin. The maxillary anteriors could then be position for optimal restoration of #11. to match the virgin #21. This is a far more extensive treatment plan but it would give us the optimal result.
I obtained a consult from a periodontist in my building about the possibility of Perio Crown lengthening. She said that she would like to try to avoid any attempted Crown lengthening procedures on the palatal aspect of #11 because of the amount of hard and soft tissue loss that would need to take place to properly Crown lengthen the tooth. Furthermore she said we may compromise the adjacent papilla should we get recession after the surgery . In THAT case, Endo treatment would be CONTRAINDICATED.
#3 – Extraction and implant replacement
Lastly, we could extract the tooth and place an implant but that still leaves us with the crowding issue.
By the time we pay for the implant we probably could have had Orthodontic treatment/forced eruption and restore #11 optimally after the Endo.
I suggested that the referring dentist create some study models and consult with an Orthodontist to see how to restore this tooth in a manner that is acceptable to the patient in the way of aesthetics, time, and cost.
Treatment Planning a Trauma Case
This 23 year old patient was seen for examination regarding tooth #11 -the maxillary central incisor. The patient had a significant history of taking a high stick to the face during a hockey game . The coronal aspect of #11 was fractured (Ellis class 3 MID) during the accident. I noted a 5 millimeter probing in the area of the palatal fracture and associated draining buccal sinus. The oblique fracture is typical in that the buccal portion cracks in the mid root while the palatal extent is far subgingival – at the bone Crest. A diagnosis of chronic periodical periodontitis secondary to pulpal necrosis was made . The other maxillary and mandibular teeth tested normally to pulp tests. No other endodontic treatment was required. The patient was lucky, the accident could have resulted in more severe injury.
The determining factor as to whether we wish to restore this tooth is based more upon restorative and other factors rather than endodontic factors. There are three factors that must be assessed before we decide whether to initiate Endodontic treatment and start the patient on the journey to rehabilitate the tooth.
#1. – The extent of the fracture on the palatal side
There is no question that the tooth cannot be restored as it presented. We will need to either extract it and replace it prosthetically or attempt to somehow obtain access to the fracture area to allow the restoring dentist to place an adequate palatal Crown margin after the Endo has been completed
#2 – The maxillary arch crowding
The anterior maxilla exhibits generalized tooth size/arch size discrepancy. This has resulted in rotation of the centrals about 40 degrees, which makes re-restoration of #11 challenging. In order to even out the centrals in terms of mesial distal width, the restoring dentist would probably have to slice or veneer the virgin #21. Either way, the restored centrals will have reduced mesial-distal width and less than optimal aesthetics.
The ideal scenario would be to place maxillary full arch orthodontics, optimally align the centrals and the rotated cuspid #23,. Ortho hardware would also allow us to perform forced eruption of #11 after endodontics is completed in order to expose the palatal Crown margin. The maxillary anteriors could then be position for optimal restoration of #11. to match the virgin #21. This is a far more extensive treatment plan but it would give us the optimal result.
I obtained a consult from a periodontist in my building about the possibility of Perio Crown lengthening. She said that she would like to try to avoid any attempted Crown lengthening procedures on the palatal aspect of #11 because of the amount of hard and soft tissue loss that would need to take place to properly Crown lengthen the tooth. Furthermore she said we may compromise the adjacent papilla should we get recession after the surgery . In THAT case, Endo treatment would be CONTRAINDICATED.
#3 – Extraction and implant replacement
Lastly, we could extract the tooth and place an implant but that still leaves us with the crowding issue.
By the time we pay for the implant we probably could have had Orthodontic treatment/forced eruption and restore #11 optimally after the Endo.
I suggested that the referring dentist create some study models and consult with an Orthodontist to see how to restore this tooth in a manner that is acceptable to the patient in the way of aesthetics, time, and cost.
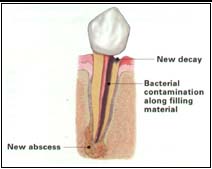
Figure: Recurrent Decay
Recurrent decay contaminates previous treatment.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Vestibulum vel dui nec elit lobortis ultricies. Proin convallis tempus est et placerat. Donec dapibus felis sed ultricies suscipit. Cras aliquet malesuada risus nec gravida.
Nullam enim quam, tristique vel congue id, cursus eu tortor. Etiam aliquet, velit non sodales cursus, massa mauris aliquam ligula, a pharetra ipsum est vel nulla. Nulla accumsan neque sit amet scelerisque eleifend.
Ut eu placerat tortor, et posuere diam. Phasellus sollicitudin dolor nec enim mattis mattis. Interdum et malesuada fames ac ante ipsum primis in faucibus.
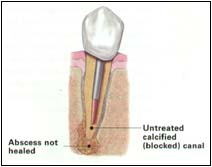
Figure: Block Canal
Endodontic failure due to Blocked Canal.