Where is YOUR Treatment Plan?
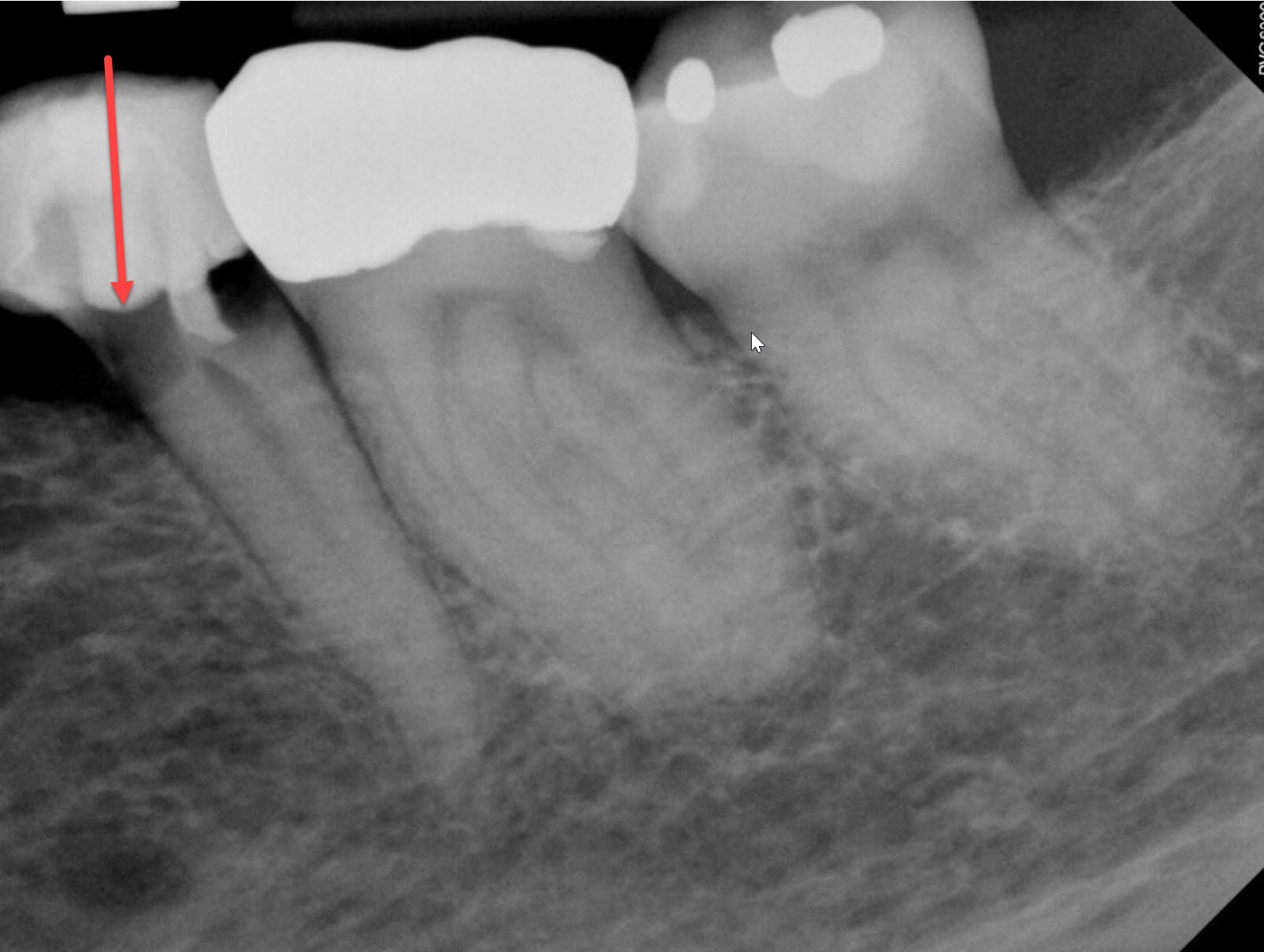
The 64 year old female patient was referred to me for possible continuation of Endodontic treatment of a mandibular 2nd premolar. The patient was referred with a note that said “Endo tx #35 – Tooth has been prepped crown ready to cement. Unable to penetrate canal.” The tooth presented with evidence of temporary Crown and prior endodontic access. The tooth was very heavily tilted, which contributed to difficulties in accessing the chamber and canal.


The patient was asymptomatic. Examination of the tooth showed that the access had been perforated the mesial part of the root. The referral documents did not indicate that the Dentist had mentioned this procedural error to the patient prior to referral.
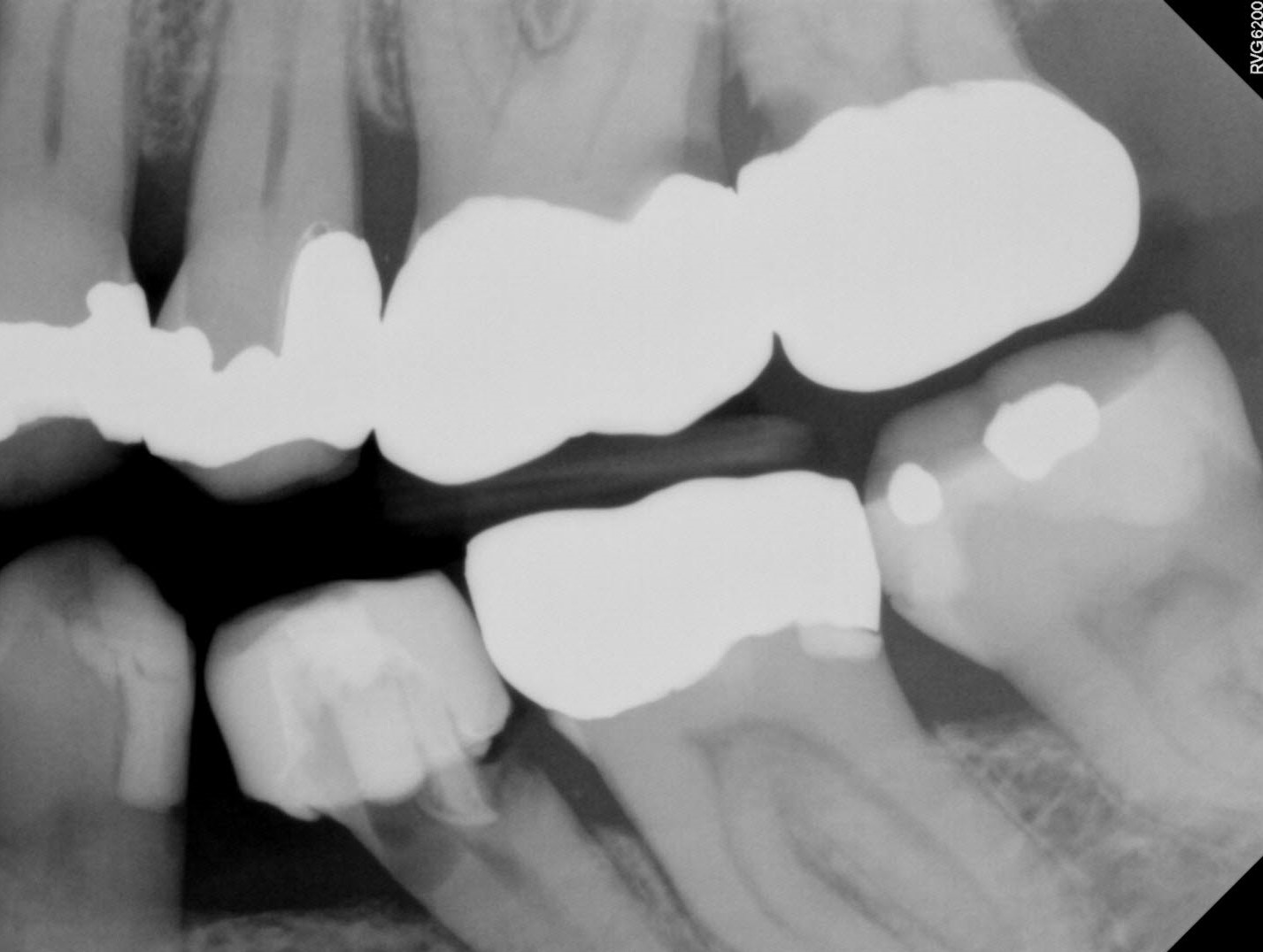
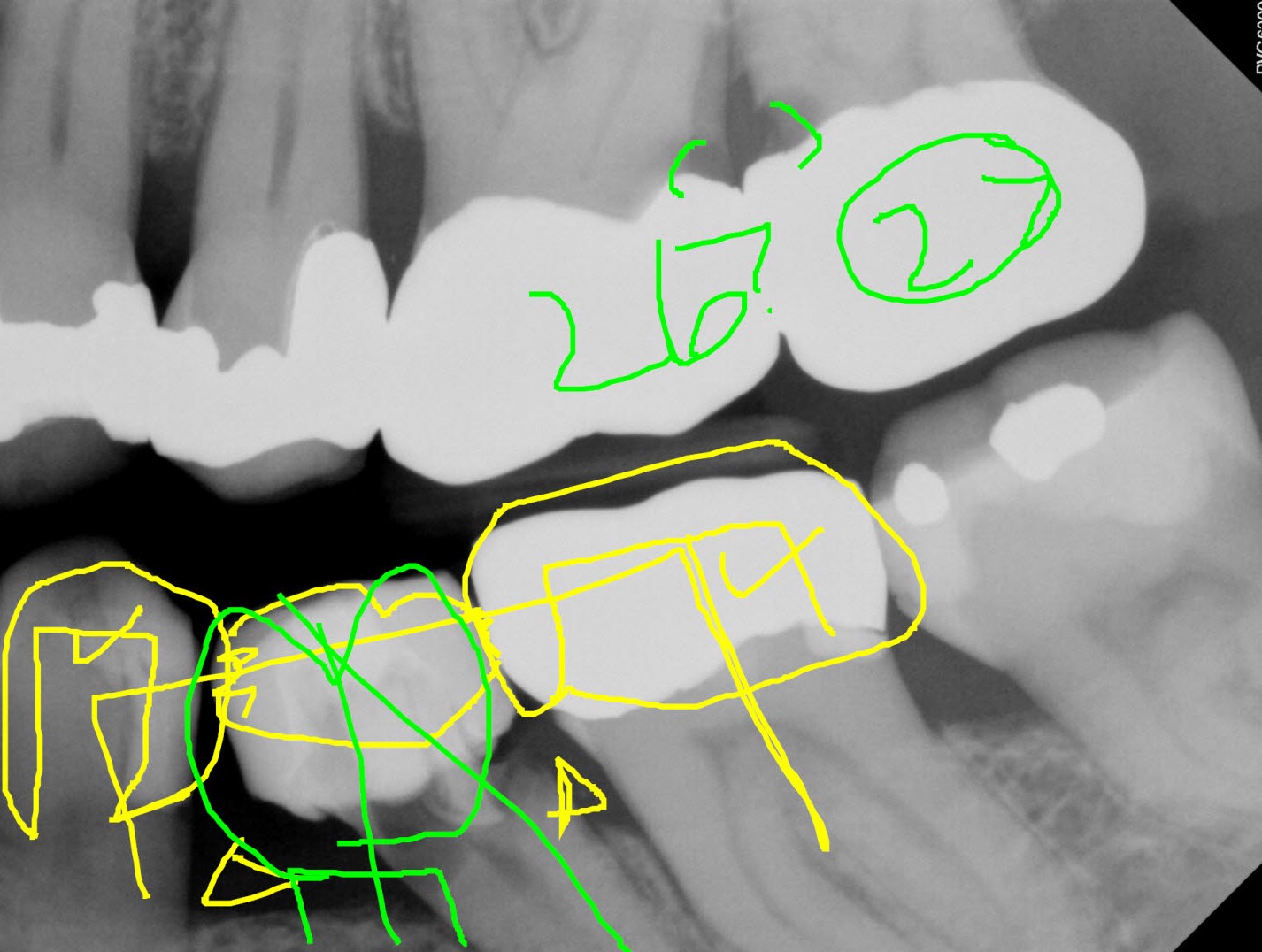
Radiographic examination showed extensive decay on the distal aspect of the tooth and access perforation on the mesial aspect of the tooth. Periapical radiography revealed extensive loss of tooth structure to the level approximating the bone Crest. As with all cases, we took a bitewing radiograph to further assess the occlusal scheme. I noted extensive decay on the mesial aspect of tooth #27 under the Crown margin and decay underneath the distal Crown margin of tooth #26. The decay in #27 appeared to be encroaching the pulp and was threatening endodontic involvement. There was no notation in the referral as to whether this had been discussed with the patient prior to referral for the mandibular premolar.
The question remains: What do we do with this information obtained from the bitewing radiography and what do we tell the patient?
Do we explain the procedural error to the and do we merely mention it in the report to the referring dentist without discussing it with the patient?
Do we mention it to the patient at the time of examination?
The referring dentist may not have discussed this with the patient prior to referral for the premolar so revealing this may be embarrassing to the referral.
Do we have a professional end ethical obligation have to discuss our findings with patients at the time they present?
The patient was referred back to their dentist for further discussions regarding a treatment plan for this area. The treatment plan implications for have these two other maxillary molars are significant. Ideally, both Crowns should be removed, the decay explored and endodontic treatment, if necessary, should be initiated.
It is my opinion that tooth #27 will probably require elective Endodontics due to the proximity of the decay to the pulp. Tooth #26 may not require Endododntics, however radiographs only show 60 to 70% of the decay that may be present in the mouth and the patient may require treatment of #26 as well, depending upon the response of the pulp to further Crown preparation.
So we can see from this that the initial Endodontic consultation for the premolar may go from a treatment plan that costs roughly $4-5000 (Extraction and implant or bridge replacement) to which may include a further $6,00-7000, depending upon whether or not these Maxillary Molars require Endodontic treatment prior to re-restoration. Since most patients do not have an unlimited budget, I believe that all of these factors must be considered before formulating a treatment plan for the left side of the mouth. (For most, the fact their insurance benefits may cover at least PART or the bridge replacement of #35 will play an important role in the decision.)
In this case that may involve initial extraction of the premolar and then temporization of both #26 and 27 until the patient can decide whether either or both of these teeth will be rehabilitated and how #35 will be replaced.
it is my opinion that the Endodontist is not only responsible for Endodontic treatment on the referred case but also for being part of the overall treatment plan and reinforcing the referring dentists treatment plan in the eyes of the patient.
This can only happen when a treatment plan is sent along with the referral, so that the patient and the referral specialist understand what the general dentist has in mind. The specialist can reinforce that message and treatment plan in the mind of the patient, ensuring that there is no possibility of saying something to the patient that maybe inconsistent, contradictory or embarrassing to the referring Dentist dentist.
The question remains: What do we do with this information obtained from the bitewing radiography and what do we tell the patient?
Do we explain the procedural error to the and do we merely mention it in the report to the referring dentist without discussing it with the patient?
Do we mention it to the patient at the time of examination?
The referring dentist may not have discussed this with the patient prior to referral for the premolar so revealing this may be embarrassing to the referral.
Do we have a professional end ethical obligation have to discuss our findings with patients at the time they present?
In this case, the premolar was deemed unrestorable and continuation of Endodontic treatment was not indicated. At that point the patient inquired as to options and we discussed both fixed bridge replacement as well as implant replacement of the premolar.
The patient was referred back to their dentist for further discussions regarding a treatment plan for this area. The treatment plan implications for have these two other maxillary molars are significant. Ideally, both Crowns should be removed, the decay explored and endodontic treatment, if necessary, should be initiated.
It is my opinion that tooth #27 will probably require elective Endodontics due to the proximity of the decay to the pulp. Tooth #26 may not require Endododntics, however radiographs only show 60 to 70% of the decay that may be present in the mouth and the patient may require treatment of #26 as well, depending upon the response of the pulp to further Crown preparation.
So we can see from this that the initial Endodontic consultation for the premolar may go from a treatment plan that costs roughly $4-5000 (Extraction and implant or bridge replacement) to which may include a further $6,00-7000, depending upon whether or not these Maxillary Molars require Endodontic treatment prior to re-restoration. Since most patients do not have an unlimited budget, I believe that all of these factors must be considered before formulating a treatment plan for the left side of the mouth. (For most, the fact their insurance benefits may cover at least PART or the bridge replacement of #35 will play an important role in the decision.)
In this case that may involve initial extraction of the premolar and then temporization of both #26 and 27 until the patient can decide whether either or both of these teeth will be rehabilitated and how #35 will be replaced.
it is my opinion that the Endodontist is not only responsible for Endodontic treatment on the referred case but also for being part of the overall treatment plan and reinforcing the referring dentists treatment plan in the eyes of the patient.
This can only happen when a treatment plan is sent along with the referral, so that the patient and the referral specialist understand what the general dentist has in mind. The specialist can reinforce that message and treatment plan in the mind of the patient, ensuring that there is no possibility of saying something to the patient that maybe inconsistent, contradictory or embarrassing to the referring Dentist dentist.
Where is YOUR Treatment Plan?
The 64 year old female patient was referred to me for possible continuation of Endodontic treatment of a mandibular 2nd premolar. The patient was referred with a note that said “Endo tx #35 – Tooth has been prepped crown ready to cement. Unable to penetrate canal.” The tooth presented with evidence of temporary Crown and prior endodontic access. The tooth was very heavily tilted, which contributed to difficulties in accessing the chamber and canal.
The patient was asymptomatic. Examination of the tooth showed that the access had been perforated the mesial part of the root. The referral documents did not indicate that the Dentist had mentioned this procedural error to the patient prior to referral.
Radiographic examination showed extensive decay on the distal aspect of the tooth and access perforation on the mesial aspect of the tooth. Periapical radiography revealed extensive loss of tooth structure to the level approximating the bone Crest. As with all cases, we took a bitewing radiograph to further assess the occlusal scheme. I noted extensive decay on the mesial aspect of tooth #27 under the Crown margin and decay underneath the distal Crown margin of tooth #26. The decay in #27 appeared to be encroaching the pulp and was threatening endodontic involvement. There was no notation in the referral as to whether this had been discussed with the patient prior to referral for the mandibular premolar.
The question remains: What do we do with this information obtained from the bitewing radiography and what do we tell the patient?
Do we explain the procedural error to the and do we merely mention it in the report to the referring dentist without discussing it with the patient?
Do we mention it to the patient at the time of examination?
The referring dentist may not have discussed this with the patient prior to referral for the premolar so revealing this may be embarrassing to the referral.
Do we have a professional end ethical obligation have to discuss our findings with patients at the time they present?
In this case, the premolar was deemed unrestorable and continuation of Endodontic treatment was not indicated. At that point the patient inquired as to options and we discussed both fixed bridge replacement as well as implant replacement of the premolar.
The patient was referred back to their dentist for further discussions regarding a treatment plan for this area. The treatment plan implications for have these two other maxillary molars are significant. Ideally, both Crowns should be removed, the decay explored and endodontic treatment, if necessary, should be initiated.
It is my opinion that tooth #27 will probably require elective Endodontics due to the proximity of the decay to the pulp. Tooth #26 may not require Endododntics, however radiographs only show 60 to 70% of the decay that may be present in the mouth and the patient may require treatment of #26 as well, depending upon the response of the pulp to further Crown preparation.
So we can see from this that the initial Endodontic consultation for the premolar may go from a treatment plan that costs roughly $4-5000 (Extraction and implant or bridge replacement) to which may include a further $6,00-7000, depending upon whether or not these Maxillary Molars require Endodontic treatment prior to re-restoration. Since most patients do not have an unlimited budget, I believe that all of these factors must be considered before formulating a treatment plan for the left side of the mouth. (For most, the fact their insurance benefits may cover at least PART or the bridge replacement of #35 will play an important role in the decision.)
In this case that may involve initial extraction of the premolar and then temporization of both #26 and 27 until the patient can decide whether either or both of these teeth will be rehabilitated and how #35 will be replaced.
it is my opinion that the Endodontist is not only responsible for Endodontic treatment on the referred case but also for being part of the overall treatment plan and reinforcing the referring dentists treatment plan in the eyes of the patient.
This can only happen when a treatment plan is sent along with the referral, so that the patient and the referral specialist understand what the general dentist has in mind. The specialist can reinforce that message and treatment plan in the mind of the patient, ensuring that there is no possibility of saying something to the patient that maybe inconsistent, contradictory or embarrassing to the referring Dentist dentist.
Where is YOUR Treatment Plan?
The 64 year old female patient was referred to me for possible continuation of Endodontic treatment of a mandibular 2nd premolar. The patient was referred with a note that said “Endo tx #35 – Tooth has been prepped crown ready to cement. Unable to penetrate canal.” The tooth presented with evidence of temporary Crown and prior endodontic access. The tooth was very heavily tilted, which contributed to difficulties in accessing the chamber and canal.
The patient was asymptomatic. Examination of the tooth showed that the access had been perforated the mesial part of the root. The referral documents did not indicate that the Dentist had mentioned this procedural error to the patient prior to referral.
Radiographic examination showed extensive decay on the distal aspect of the tooth and access perforation on the mesial aspect of the tooth. Periapical radiography revealed extensive loss of tooth structure to the level approximating the bone Crest. As with all cases, we took a bitewing radiograph to further assess the occlusal scheme. I noted extensive decay on the mesial aspect of tooth #27 under the Crown margin and decay underneath the distal Crown margin of tooth #26. The decay in #27 appeared to be encroaching the pulp and was threatening endodontic involvement. There was no notation in the referral as to whether this had been discussed with the patient prior to referral for the mandibular premolar.
The question remains: What do we do with this information obtained from the bitewing radiography and what do we tell the patient?
Do we explain the procedural error to the and do we merely mention it in the report to the referring dentist without discussing it with the patient?
Do we mention it to the patient at the time of examination?
The referring dentist may not have discussed this with the patient prior to referral for the premolar so revealing this may be embarrassing to the referral.
Do we have a professional end ethical obligation have to discuss our findings with patients at the time they present?
In this case, the premolar was deemed unrestorable and continuation of Endodontic treatment was not indicated. At that point the patient inquired as to options and we discussed both fixed bridge replacement as well as implant replacement of the premolar.
The patient was referred back to their dentist for further discussions regarding a treatment plan for this area. The treatment plan implications for have these two other maxillary molars are significant. Ideally, both Crowns should be removed, the decay explored and endodontic treatment, if necessary, should be initiated.
It is my opinion that tooth #27 will probably require elective Endodontics due to the proximity of the decay to the pulp. Tooth #26 may not require Endododntics, however radiographs only show 60 to 70% of the decay that may be present in the mouth and the patient may require treatment of #26 as well, depending upon the response of the pulp to further Crown preparation.
So we can see from this that the initial Endodontic consultation for the premolar may go from a treatment plan that costs roughly $4-5000 (Extraction and implant or bridge replacement) to which may include a further $6,00-7000, depending upon whether or not these Maxillary Molars require Endodontic treatment prior to re-restoration. Since most patients do not have an unlimited budget, I believe that all of these factors must be considered before formulating a treatment plan for the left side of the mouth. (For most, the fact their insurance benefits may cover at least PART or the bridge replacement of #35 will play an important role in the decision.)
In this case that may involve initial extraction of the premolar and then temporization of both #26 and 27 until the patient can decide whether either or both of these teeth will be rehabilitated and how #35 will be replaced.
it is my opinion that the Endodontist is not only responsible for Endodontic treatment on the referred case but also for being part of the overall treatment plan and reinforcing the referring dentists treatment plan in the eyes of the patient.
This can only happen when a treatment plan is sent along with the referral, so that the patient and the referral specialist understand what the general dentist has in mind. The specialist can reinforce that message and treatment plan in the mind of the patient, ensuring that there is no possibility of saying something to the patient that maybe inconsistent, contradictory or embarrassing to the referring Dentist dentist.
