Two Rooted Central – Treat or not?
This patient was sent to me because of persistent sensitivity to percussion associated with previous Endo treatment of this maxillary central incisor.
Radiographically the Endodontic filling looked a bit “skinny” and there appeared to be slight over extension . The canal appeared under-prepared and it was probably obturated with lateral condensation, as we can see by the clinical appearance of the filling material in the radiograph. There are some voids in the fill as well. A small lateral radiolucency is visible along the distal aspect of the tooth at the mid root level. Examination of a second off angle film shows a small radiolucent area at the apex.
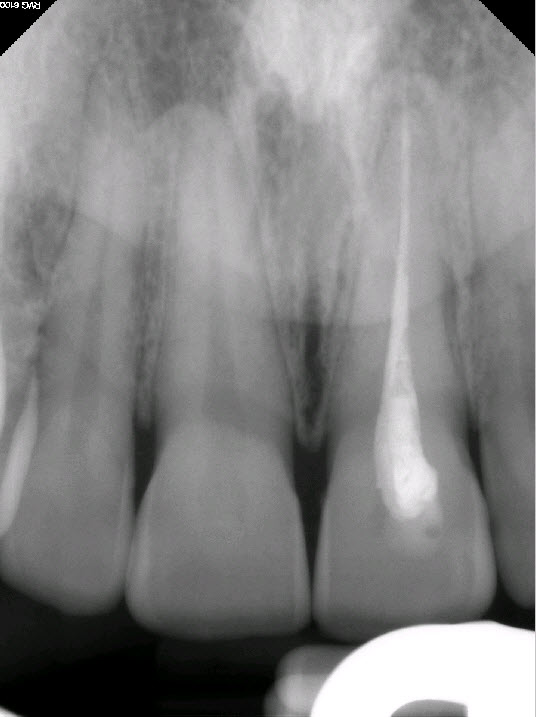
Figure 1: Periapical Radiograph 1
Slightly long fill, voids in filling, likely lateral condensation.
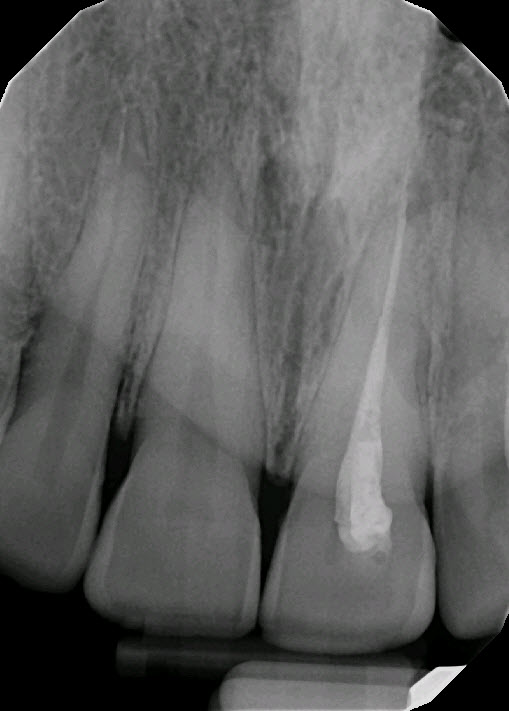
Figure 2: Periapical radiograph 2
Possible lateral radiolucency at Distal midroot and apex.
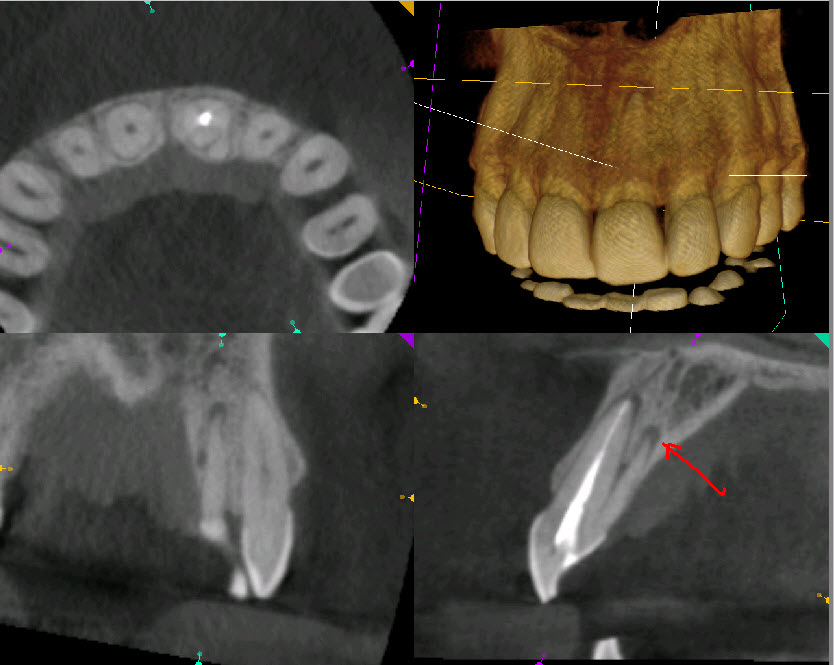
Examination of the labial gingiva shows no evidence of a draining buccal sinus. The tooth is slightly discolored but other than that it looks fairly normal. Percussion was very slightly positive and palpation was negative. Periodontal examination of the palatal side of the tooth give a hint of what the problem may have been. If we compare the two central incisors, we notice that the left central has a slight groove on the palatal surface similar to that of the the adjacent lateral incisors. Periodontal probing of the palatal gingiva yielded about a 6 millimeter pocket. I decided to take a cone beam tomograph to further examine the tooth from a proximal view. I immediately noted the presence of a second palatal root and associated apical radiolucent findings in both roots.

Figure 3 : Maxillary Central Incisor
Slight discoloration but no other visible findings
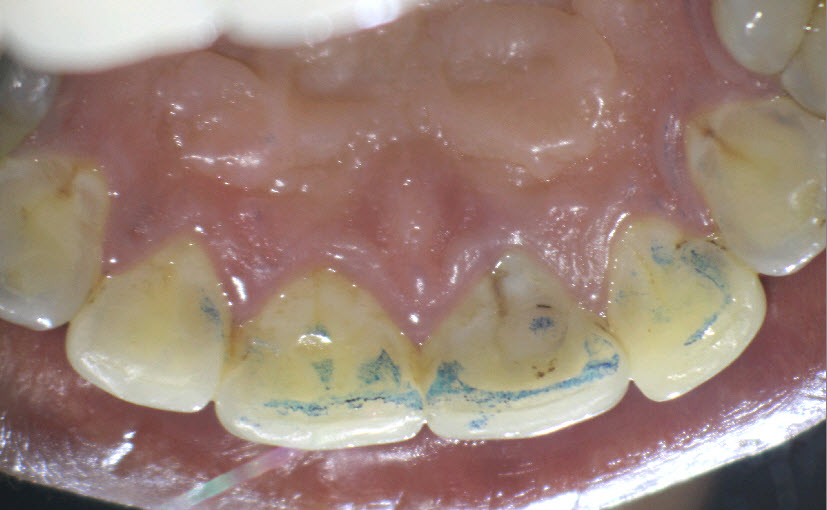
Figure 4: Palatal view
Note discolored, stained groove on palatal aspect
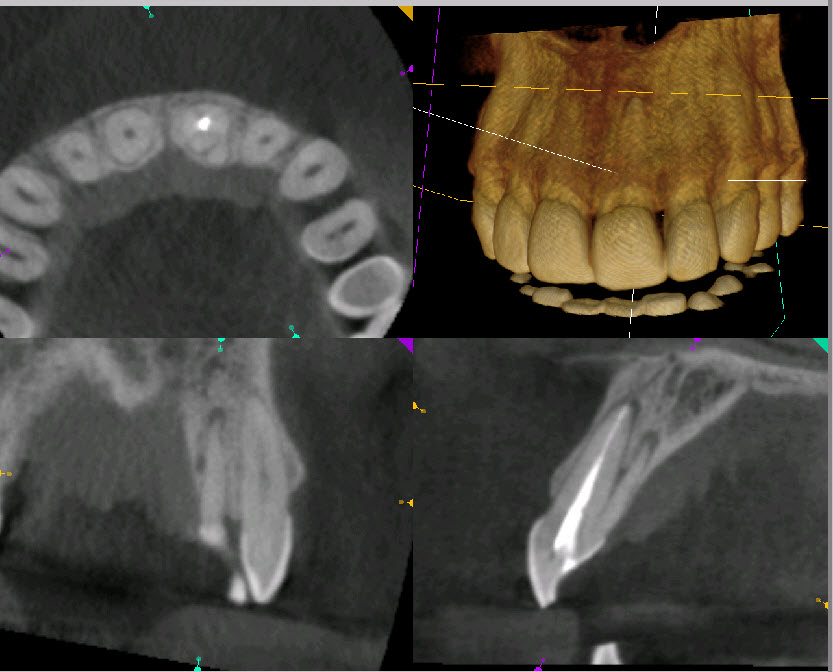
Figure 5: Proximal View
Scan shows second Palatal root with no visible canal
Clinical management of the case proved to be a real challenge. Because of the small size of the second palatal root, there appeared to be literally no canal visible, as seen in the cbCT scan. Attempting to access this root to find a canal ran the risk of perforation and ruining what was (in the opinion of the patient) a perfectly good tooth. Retrograde surgery was ruled out because a buccal approach to surgery would sacrifice too much of the buccal root during resection, so this was not feasible. Another possibility we considered was to apically resect or remove the additional palatal root entirely. While Resection of the extra palatal root would eliminate it, the remaining exposed, resected palatal root dentin would have no cementum on it and would not attach to the palatal gingiva. That approach would likely result in significant palatal bone loss, persistent pocketing and likely compromise of the support on the palatal side of the tooth.
Ultimately, we decided that no treatment was the best option. Symptoms were minimal and certainly did not justify such an extensive surgical intervention. Sometimes it is best to leave situations like this alone, when patients are minimally symptomatic, and further treatment of the area risks loss of the tooth or making the situation worse.
This is an excellent example of “Disease versus Disease that Matters”. Is there a periapical radiolucent finding that indicates incomplete healing? Yes. Does that merit treatment? In, this case, no. Clinical judgment and assessment of the patients attitudes toward treatment and possible tooth loss must be considered whenever we are deciding whether to intervene or not. In this case we chose to leave the situation as is, with the consent of the patient.
Figure 6: Are there any surgical options?
Buccal surgical approach not feasible. Resection of the palatal miniroot would result in loss of palatal bone and risks loss of Perio support.