Lazy Diagnosis Misses the Mark
A 64 year old male patient was referred to me for consideration of symptoms associated with the maxillary left premolar area. Both premolars had been restored with full crowns and there appeared to be a small draining buccal sinus in between these two teeth. The patient was relatively asymptomatic and the sinus had been noted during his hygiene appointment with the referring Dentist.
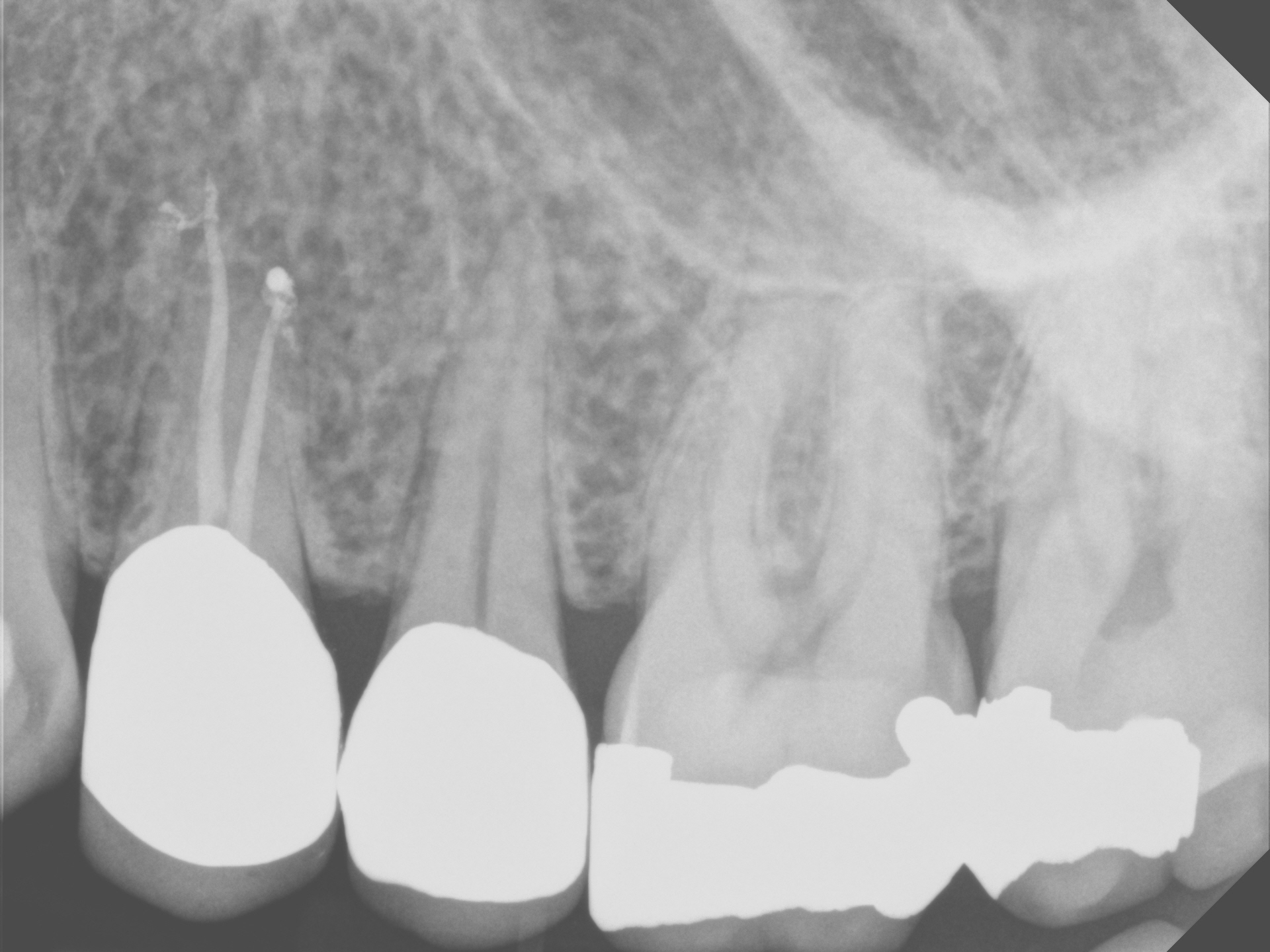
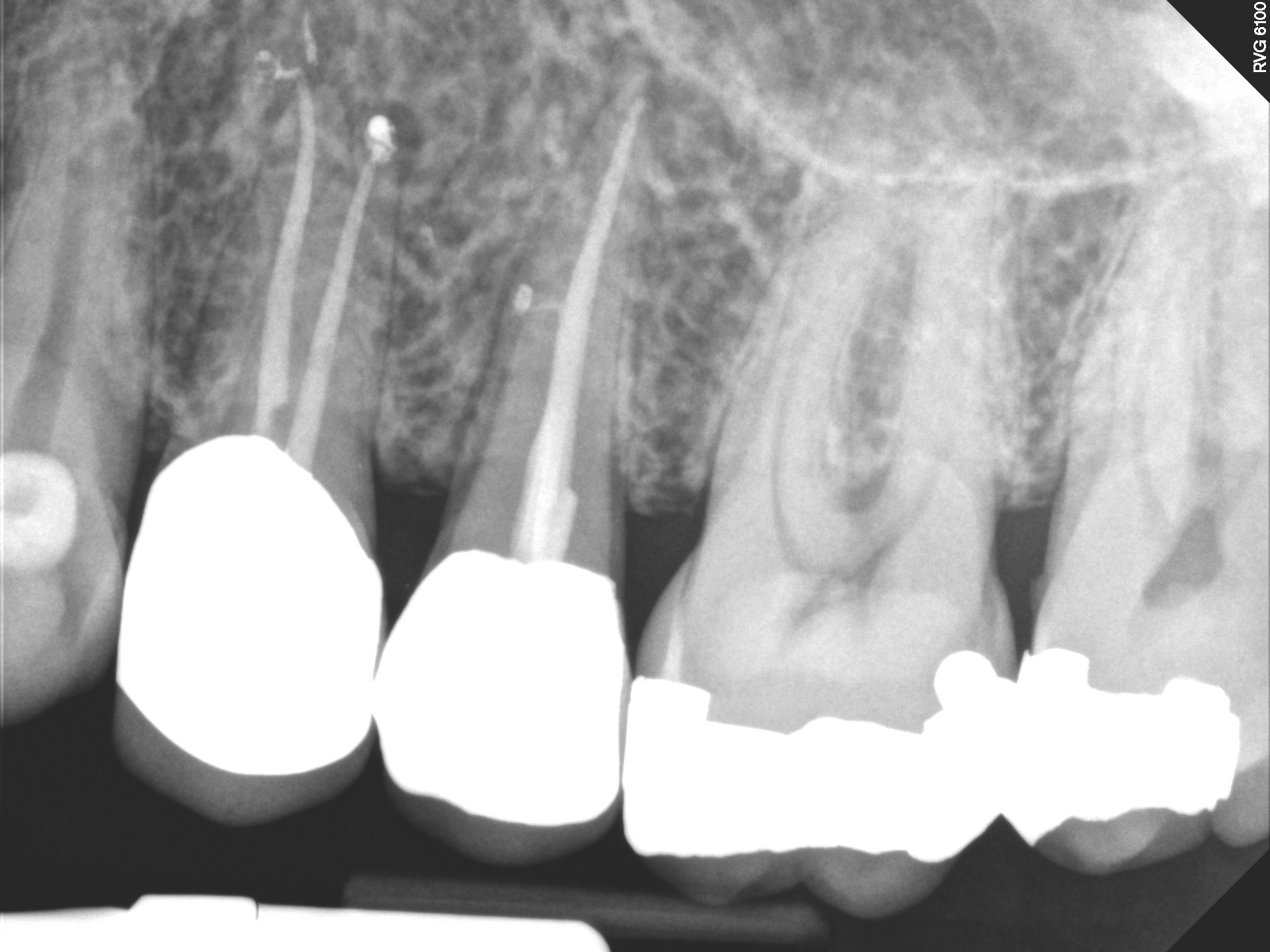
Radiographic examination revealed a radiolucent finding associated with the maxillary first premolar(#24). Cold tests performed on #24 revealed no responses. Even though the Crown may have been shielding the pulp from responses to cold tests, I felt that radiographic confirmation of the radiolucency combined with the associated draining buccal sinus likely indicated that the pulp in #24 was necrotic.



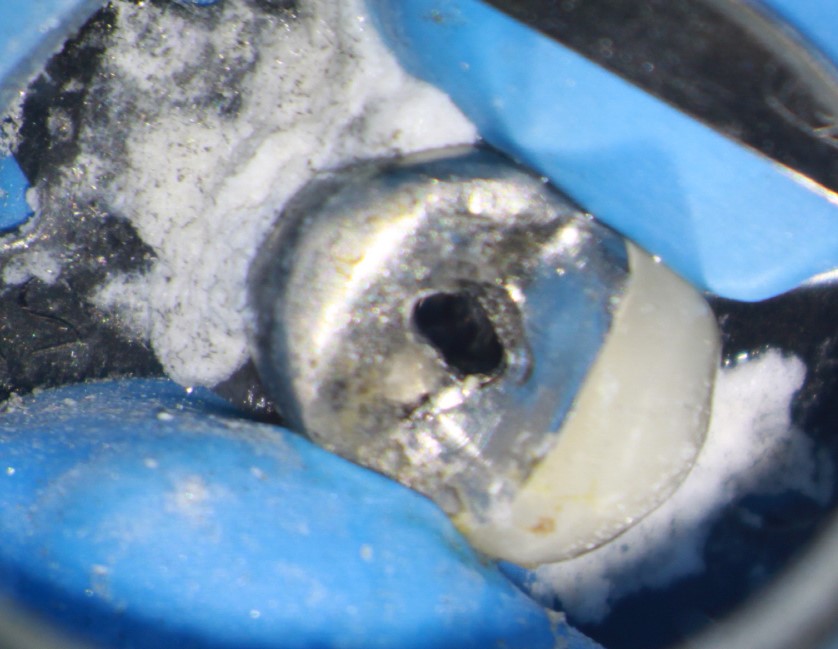
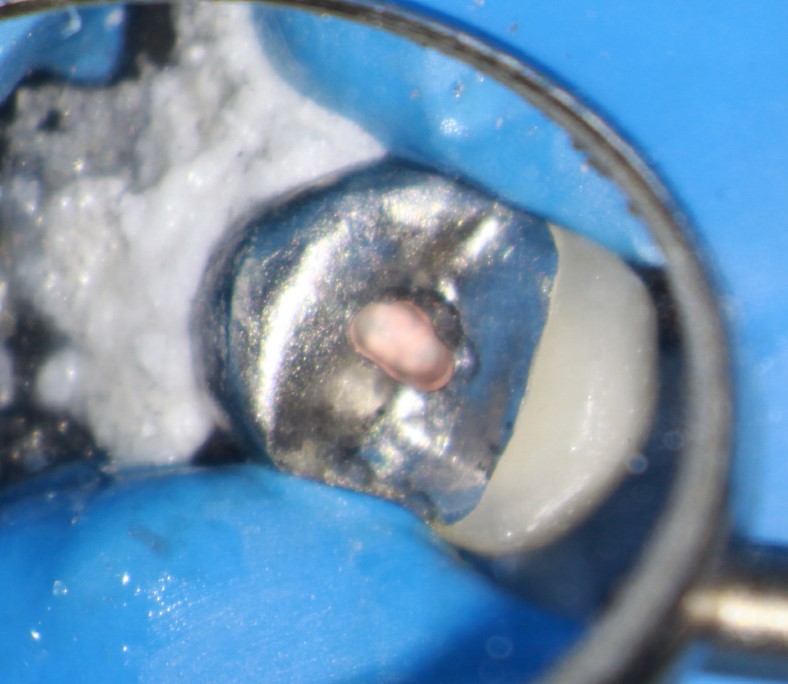
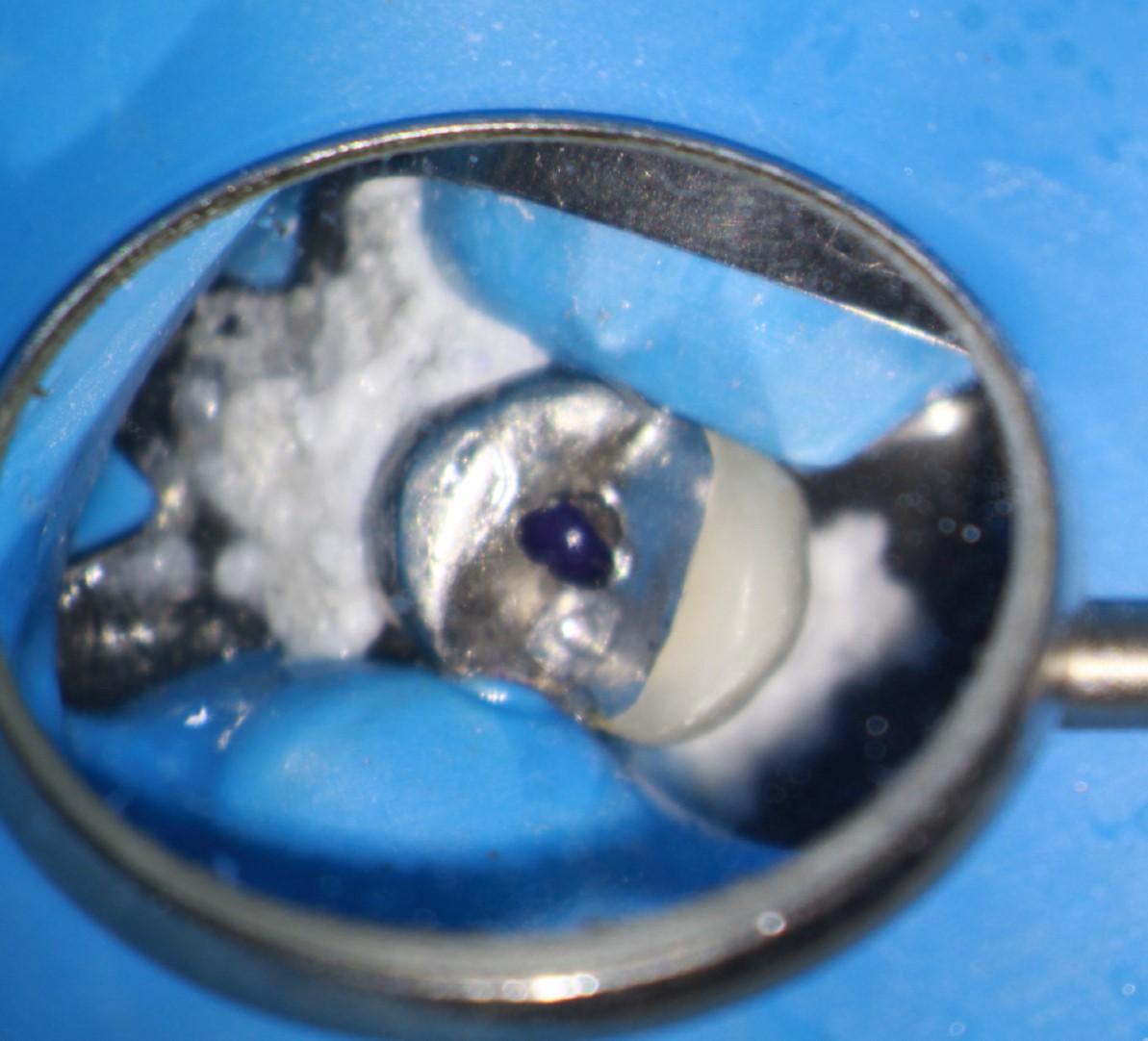
I explained my findings to the patient and we immediately put on a rubber dam and performed a cavity test (no anesthetic). Upon access into the chamber, the pulp was found to be necrotic and endodontic procedures were initiated on the tooth. Because the patient was traveling from far away, he requested he that treatment be performed in a single appointment, if possible. Endodontic treatment of this 2 canal premolar was completed and the access was closed with amalgam. I was pleased with the radiographic appearance and expected the sinus to resolve.

I was subsequently informed by the referring dentist that the draining buccal sinus had persisted and that I needed to see the patient again. I was a bit puzzled that the problem had not resolved because I had been fairly confident in my diagnosis and treatment results, at least radiographically.

The buccal sinus had returned, now with a slight area of swelling . At that point, I decided to take a cbCT, which revealed a radiolucent area associated with apex of the second Premolar (#25). A rubber dam was placed and another cavity test was performed, at which time I noted that the pulp in this tooth was also necrotic. Treatment was completed and the access was closed . A nice lateral canal (which appeared to be close to the sinus area) was filled in the final image. The patient’s symptoms disappeared and the problem was solved .
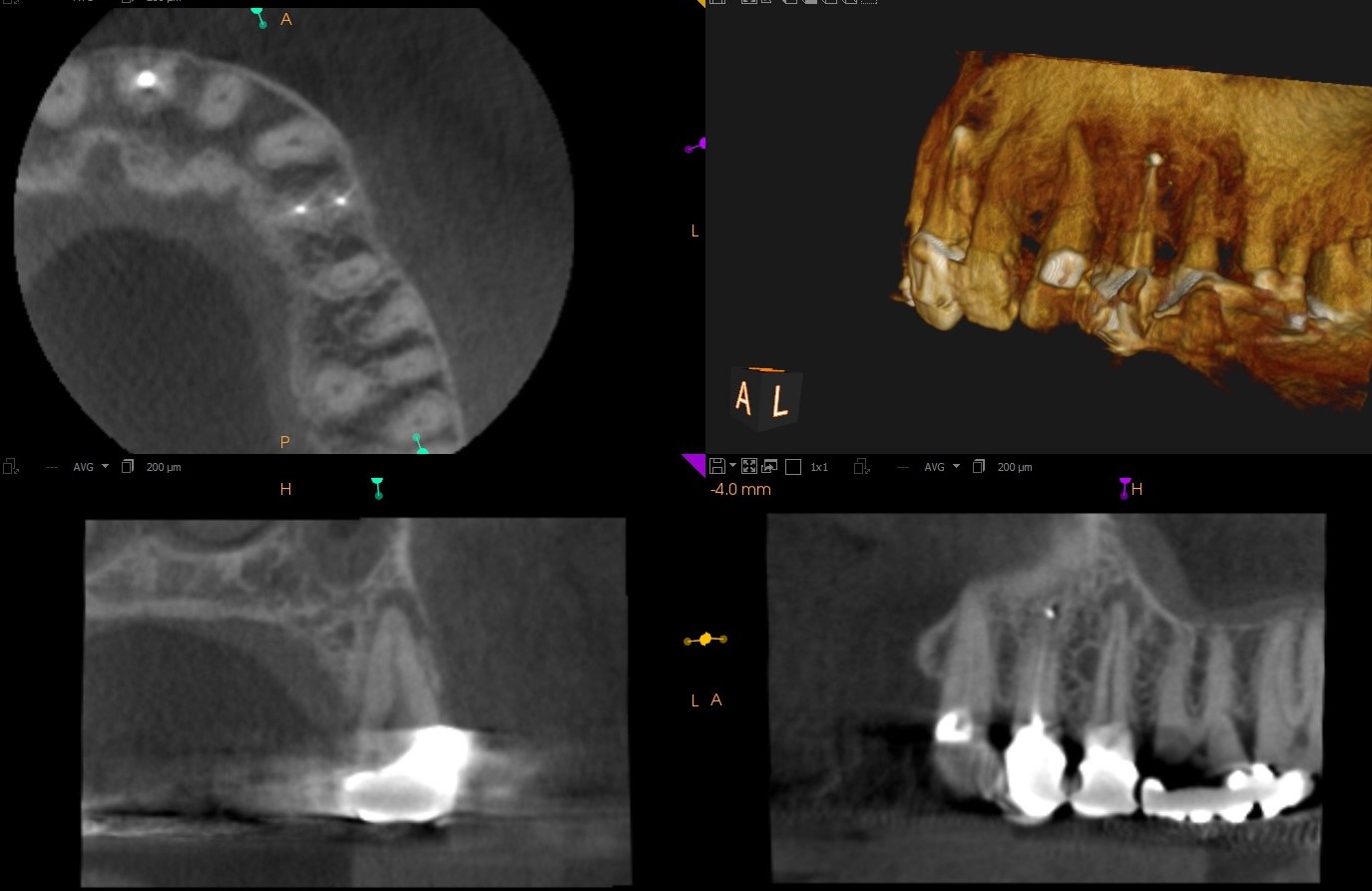
Hindsight is always 20/20. Looking back now, it probably would have been a good idea to image the area with CBCT at the onset.
The likelihood of the pulps of two adjacent premolars that had been crowned becoming necrotic at the same time is fairly low .
Furthermore the original preoperative radiograph did not show anything unusual about the periapical area associated with the second premolar #25 . The initial diagnosis seemed fairly obvious. However, in endodontics “obvious” should merely be taken as suspicious until findings are confirmed .
In this case, “lazy” diagnosis on my part caused me to miss that the draining sinus was associated with #25 rather than the first premolar #24. Had I not thought the diagnosis was so “obvious”, I may have taken steps to be more certain by:
(a) Tracing of the sinus to its source with a gutta percha cone – which would have likely pointed to #25 and
(b) Taking a cbCT image from the start – which would have confirmed that BOTH premolars required Endo treatment.
What did we learn form this case? Things are not as obvious as they may seem, when it comes to Endodontic pathology.
