Treatment Plan Considerations
Prior to Referral – Again


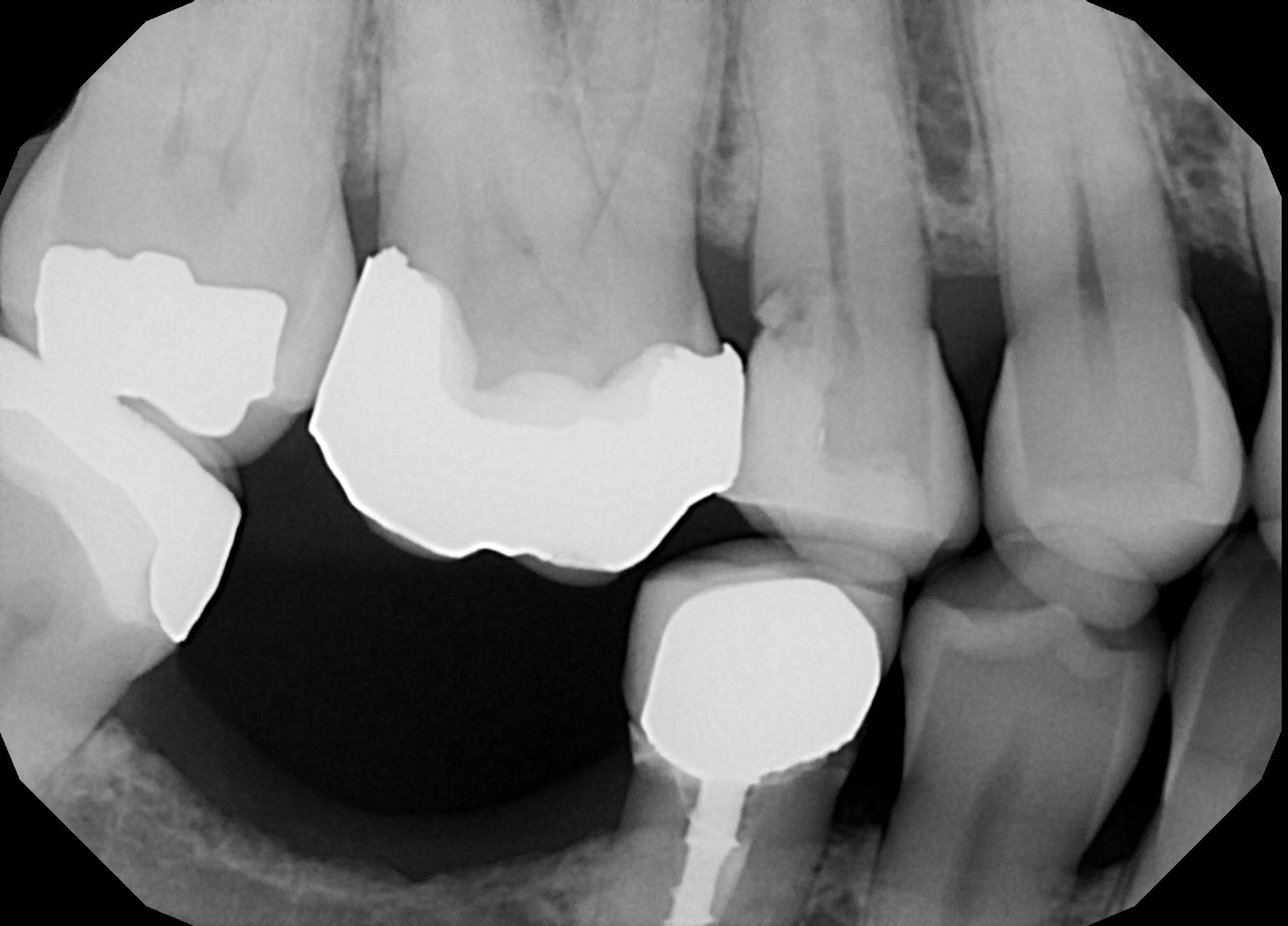

This 55 year old female patient was seen for symptoms of irreversible pulpitis in #15 and initiation of endodontic treatment. The patient presented with deep D caries to the bone crest. Prior to referral to me, I reviewed the image and consulted with the referring dentist on the phone; I was not sure whether this tooth was restorable. There was a “plunger cusp” situation caused by a combination of: #45 crown, supra-eruption of #16 and loss of #46. This is causing food impaction on the distal aspect of #15.
Upon access and excavation of the distal caries in#15, the tooth was found to have very deep decay. A Periodontist in my building was called for consultation and agreed with my findings: the tooth had questionable restorability. Even if we did attempt to crown lengthen #15, any Perio surgery could affect the furca of the supraerupted adjacent #16. Why risk losing both teeth to try to save a barely maintainable #15?
There also appeared to be some decay on the M aspect of #45, under the M crown margin.
Before initiating Endo treatment on #15, I told the referring Dentist that we needed to discuss the ultimate goals of treatment and any alternatives the patient may wish to consider. They included:
(1) Extraction of #15.
(2) Crown #16 (with or without elective endo as required) and 3 Unit Bridge #16-14
(3) Single implant to replace #46. (Done in conjunction with crown #16) OR 3 unit bridge #47-45 (depending on whether the crown in #45 needs to be remade.
As we can see, there are several options.
I removed decay to sound dentin and performed a pulpectomy to get the patient comfortable and relieve her complaint of thermal sensitivity. The tooth was temporized with a Rebilda DC DO core paste temp. I recommended that the referring dentist remove this temp and assess the case for restorability himself, or simply extract the tooth and discuss options with the patient.


There is a tendency to regard such symptomatic patients as a single procedure referral. I believe the ethical thing to do would be to have these discussions before the referral is sent out so that the patient understands the proposed procedure and all costs involved in rehabilitation of the tooth and of that side. Ideally, we would like to restore function on the right by replacing the missing mandibular first molar (#46) and possibly crowning the supraerupted maxillary first molar (#16) at the same time, restoring it back into the proper occlusal plane. We could do this in conjunction with either a single molar implant (#46) or bridge #47-45. All we needed to do was to decide on HOW to do this and get informed consent.
For some patients (especially those who must rely upon insurance benefits for their dentistry) an implant that is not covered by insurance is not a financial alternative – whereas the bridge MIGHT BE an option. -> either to replace the questionably restorable #15 OR the missing #46. Removal of the bicuspid Crown (#45) and preparation of the second mandibular molar for a 3 unit mandibular bridge is obviously not the ideal treatment, however it may be the only affordable way for this particular patient to restore the quadrant.
The whole point of this case presentation is to emphasize that the endodontist receiving such a referral without any guidance as to what the referring dentist has planned for this side, is at quite a disadvantage. The easiest thing for an endodontist to do would be simply to treat the maxillary premolar without any discussions regarding restorability, source of the decay, prosthetics or further treatment plan considerations. But is this the right thing to do for the patient? And contrast that attitude with the kind of discussions that would take place if you or your family member would be in such a situation?



