The Myth of the Apical Constriction
This mandibular first molar was referred to me for possible treatment due to the presence of a draining buccal sinus . The patient remarked that it had been there for a long time and it had never really bothered him so he never sought treatment.
The tooth was mildly percussive and showed furcation involvement on the buccal aspect. Radiographic examination showed extensive external resorption of both mesial and distal roots.

What prompted me to include this in case of the month was the concept of the apical constriction and where it could possibly be found in a case like this. Many of us learned to try to end our Endodontic filling materials at what is known as the apical constriction – short of the radiographic terminus. This is generally acknowledged to be the narrowest point before the canal exits the apex of the tooth. It is usually made of cementum and dentin or a combination of the two.
In the case of a vital pulp, the anatomy is usually not disturbed. Of course if the patient has undergone orthodontic treatment, the apices can be blunted or altered from the classic apical shape, even in a vital tooth.
In the case of a necrotic canal with periapical involvement, we know that the apex of the affected tooth usually undergoes some inflammatory resorption to a certain extent. When a chronic periapical peridontitis is left for long periods of time (such as in this case), extensive amounts of root structure can be resorbed resulting in a canal that is often wider at the apical end. Not only does this make dealing with the case challenging due to the bacterial aspect, but now we are faced with trying to confine our filling materials to the canal space.
Consulting with both the patient and the referring dentist, we came to the conclusion that the amount of root destruction and the furcation involvement (as visible on the cone beam tomograph) suggested that the prognosis was not very good overall.
We gave the patient the choice of accessing the tooth and medicating with calcium hydroxide in the hope that we could resolve the periapical inflammation and grown the bone back. However, the patient chose to have the tooth extracted and replaced with an implant rather than undergo treatment that had a less certain long term prognosis
The whole point of showing this case was to emphasize that the apical construction is a myth in most cases where pulpal necrosis and long term pathology is involved. Even in cases where the pulp is vital, anatomic studies have shown that while we may be able to find a construction, it rarely is “the” construction in almost all but the easiest of cases. Establishing the apical extent of your Endodontic filling in situations like this must be done with a combination of electronic apex location, cone beam tomography, tactile feel and paper point working length determination.
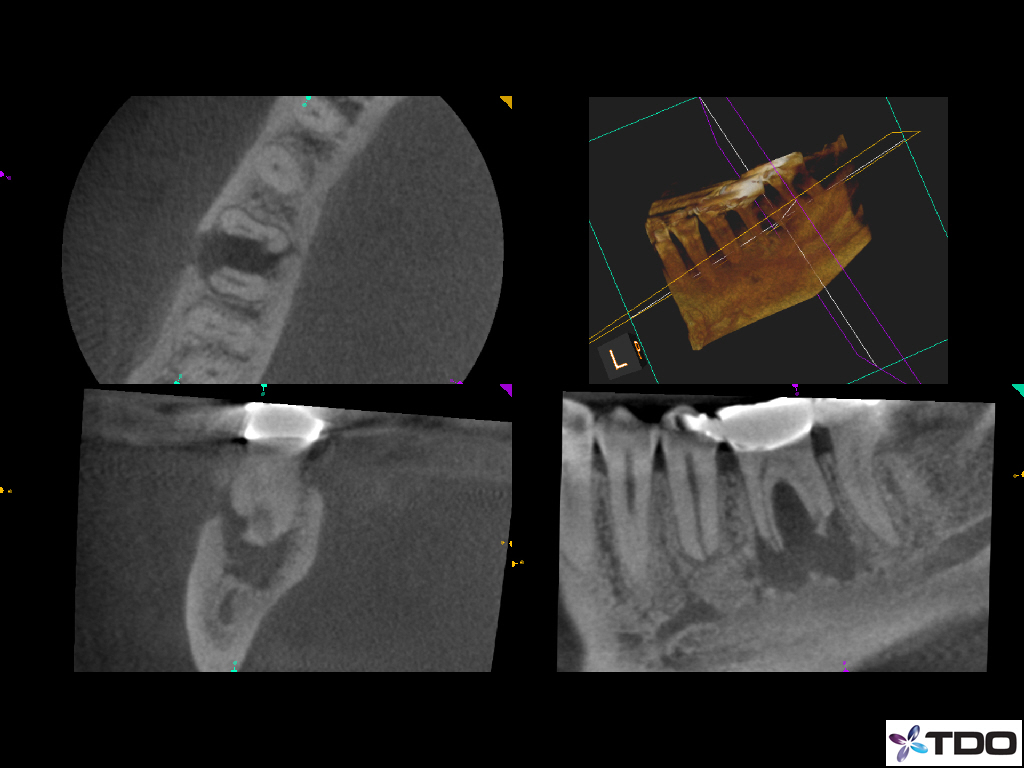
Figure 1: Extensive resorption
Where do you terminate your endo filling?
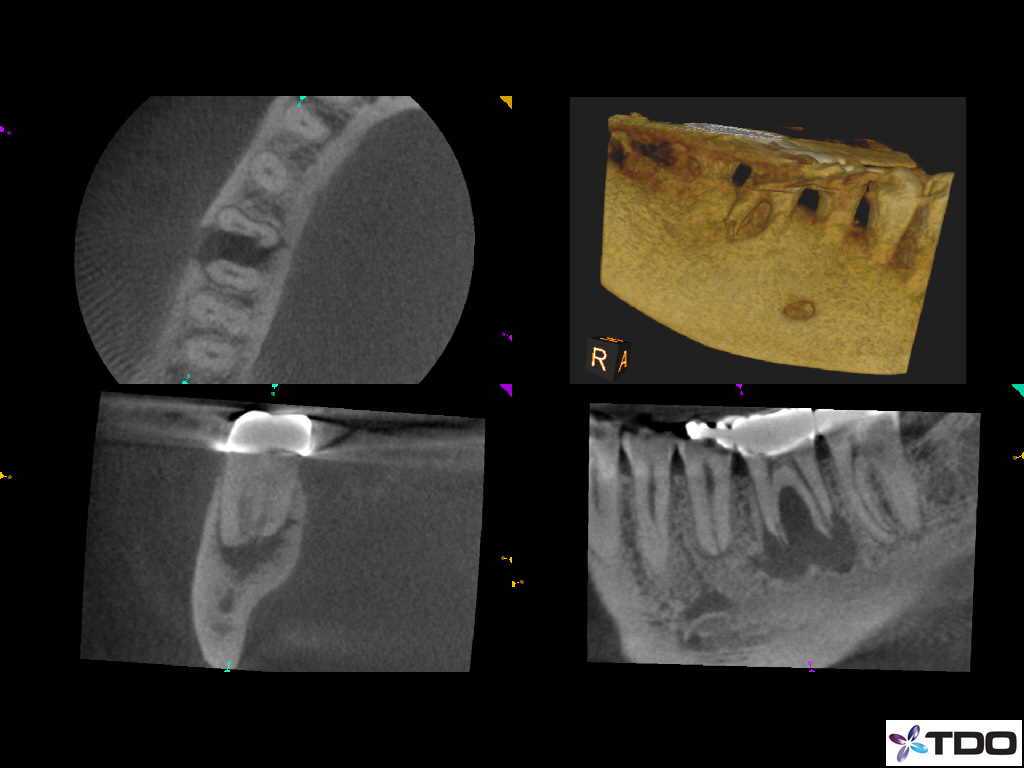
Figure 2: Extensive resorption – 2nd view
Where do you terminate your endo filling?

