Retreatments can Sometimes be Ugly
A 33 year old male patient was referred to me for possible endodontic retreatment of tooth #46. The tooth had Endodontic treatment about 7 years previously and had persistent symptoms to chewing as well as a draining buccal sinus. The referring dentist was considering placing a definitive restoration over this tooth as the tooth had not been crowned and the amalgam core margins seemed to be breaking down.


Clinical examination revealed draining buccal sinus and a 3 canal Endodontic treatment with post and amalgam core restoration. Percussion was slightly positive and Peridodontal findings were within the range of normal with the exception of the draining buccal sinus.
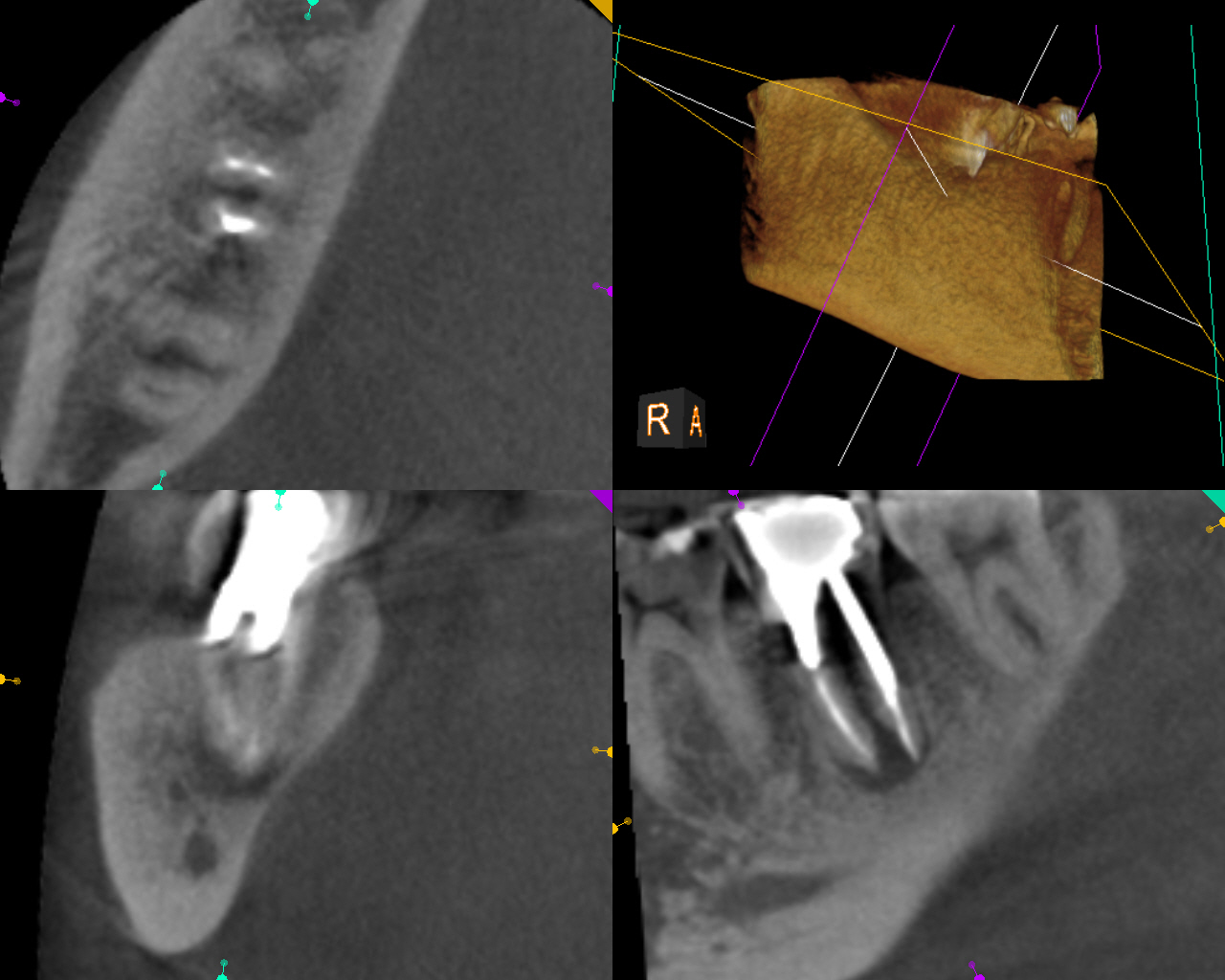
Radiographic examination showed a diffuse radiolucent area associated with the apex of the tooth. The tooth would require disassembly retreatment .
I explained to the patient that we would need to disassemble the tooth, remove the post and medicate the tooth in order to see if we could get the buccal sinus to close. Once the sinus is closed, obturation would then be performed and the tooth closed temporarily. The patient would be instructed to return immediately to their dentist for core buildup and/or final Crown restoration.
As with any re treatment case, the patient was advised that sometimes surgical procedures are required to correct the problem and we would need to assess whether the patient was willing to undergo such procedures in the event that retreatment was not successful . He agreed to the disassembly retreatment.
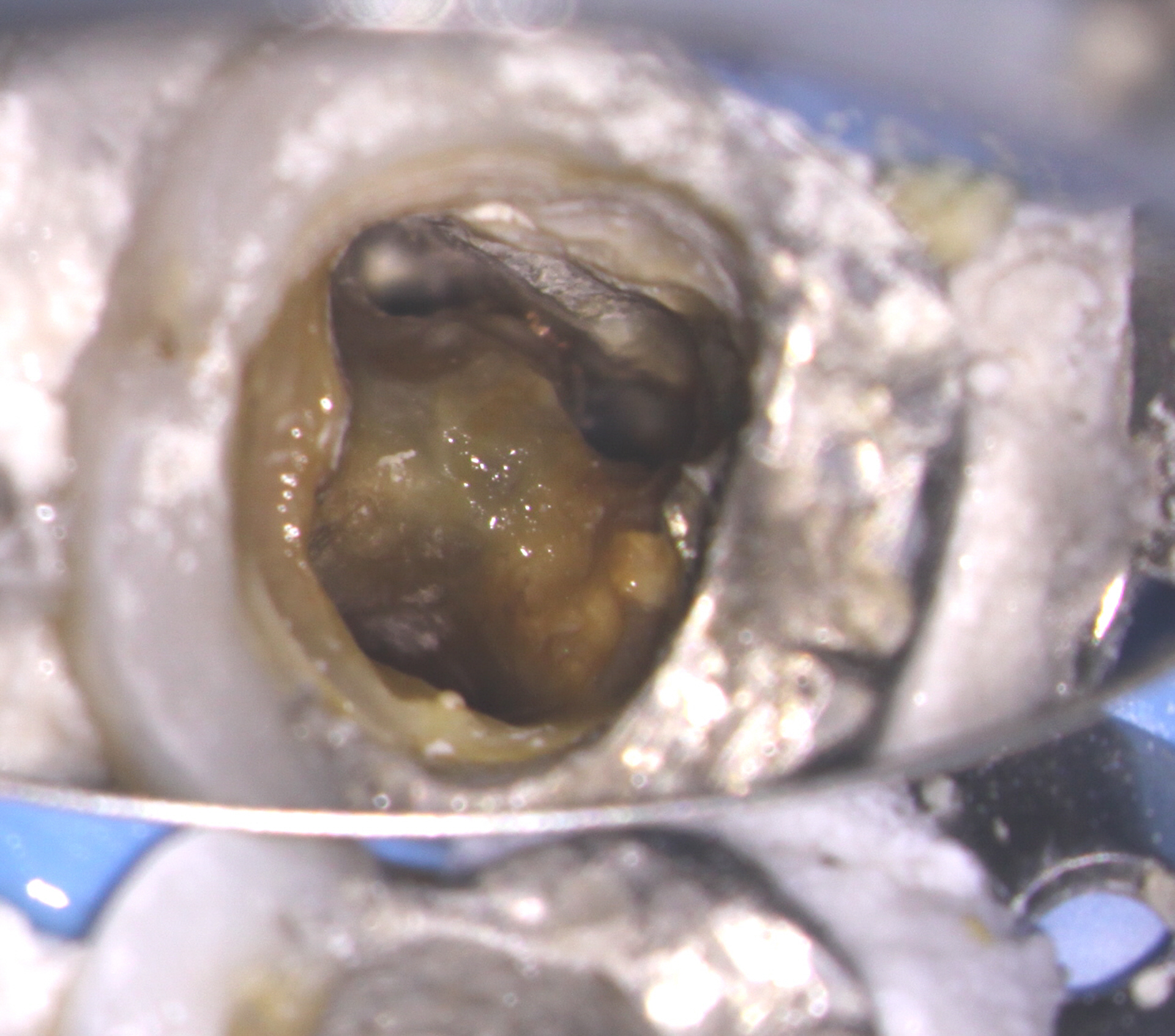
The patient was anesthetized and rubber dam placed. The core amalgam filling was removed as well as the post, which came out fairly easily. the original filling material was removed and the canals were cleaned and shaped. I was not very happy with the shapes (especially on the mesial-coronal aspect). Unfortunately there is not much you can do about previous over enlargement of the access or canals, other than to try to conserve as much tooth structure as possible during the retreatment. Calcium hydroxide medication was placed in the canals and the patient was left for three weeks.


At the 2nd appointment, the buccal sinus had closed and the case was ready for obturation. The Endo treatment was completed and the tooth was temporized. Since orifice bonding was not being used (to allow for placement of core material in the prepared retention spaces), calcium hydroxide was placed in the prepared core retention spaces to aid with asepsis in between appointments. ( I requested no posts!) The access was closed with sponges and bonded core paste temporary filling. The patient was instructed to return to their dentist immediately to have the tooth restored with a Crown.

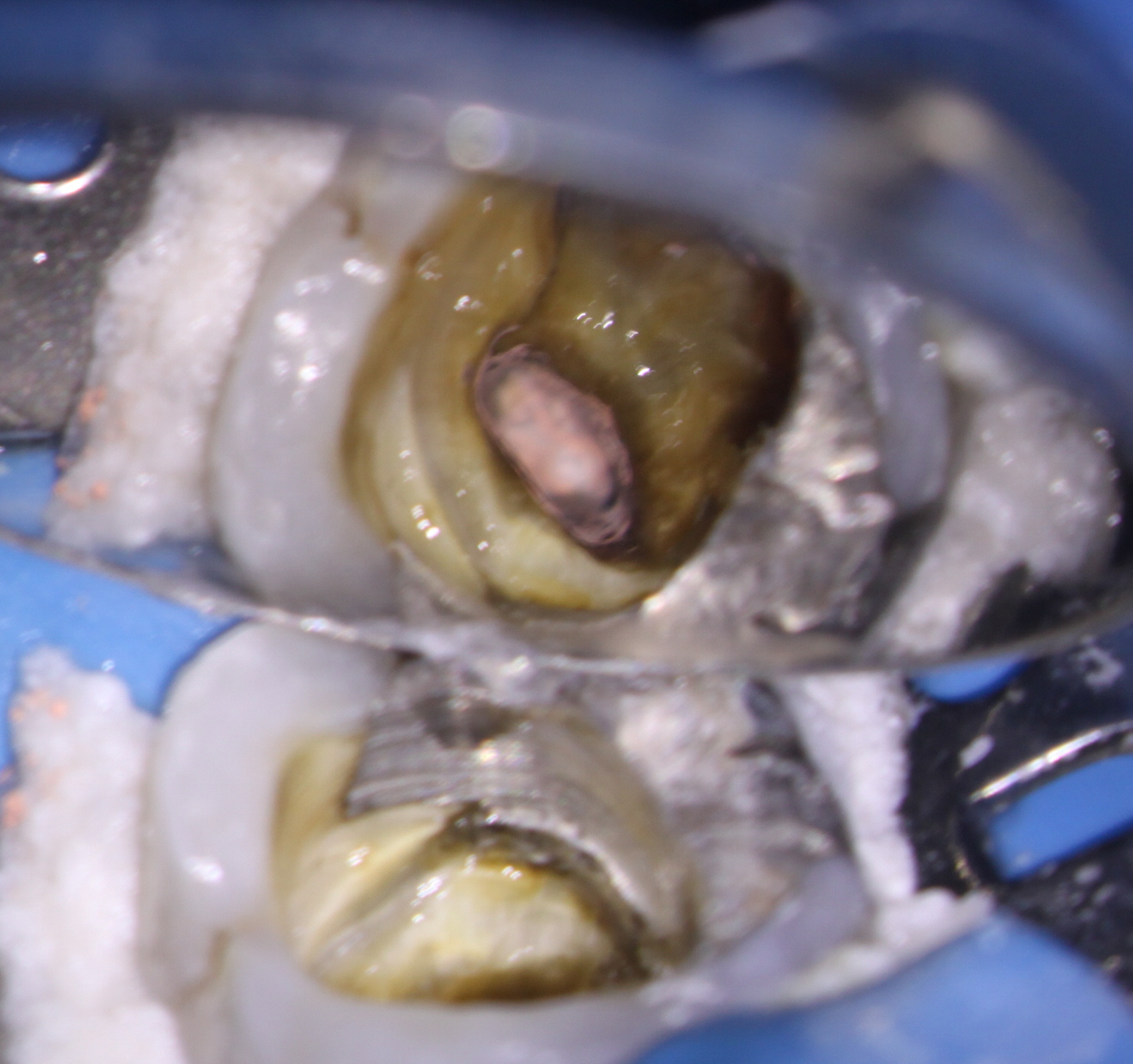

Ideally, the clinician performing endodontic treatment should place the core immediately after Endo treatment but in this case the general dentist wished to do this himself.


I was somewhat disappointed to see that at a six month recall, my original temporary filling was still in place. The periapical areas appeared to be healing well and the patient was completely asymptomatic.
A recall report was sent to the referring dentists urging them to place the final definitive restoration as soon as possible to prevent Coronal leakage or possible catastrophic fracture.
Unfortunately, when retreatments like this are done at the beginning of the calendar year, patients frequently have to wait until the next calendar year. Some do not have the financial resources and because they rely on insurance plan benefits to fund their Dentistry, they often delay final restoration. In that case, I urged the referring dentist to at least place a core restoration or temporary Crown in order to prevent the possibility of coronal leakage and/or catastrophic fracture of the tooth.

