Retreatment Options
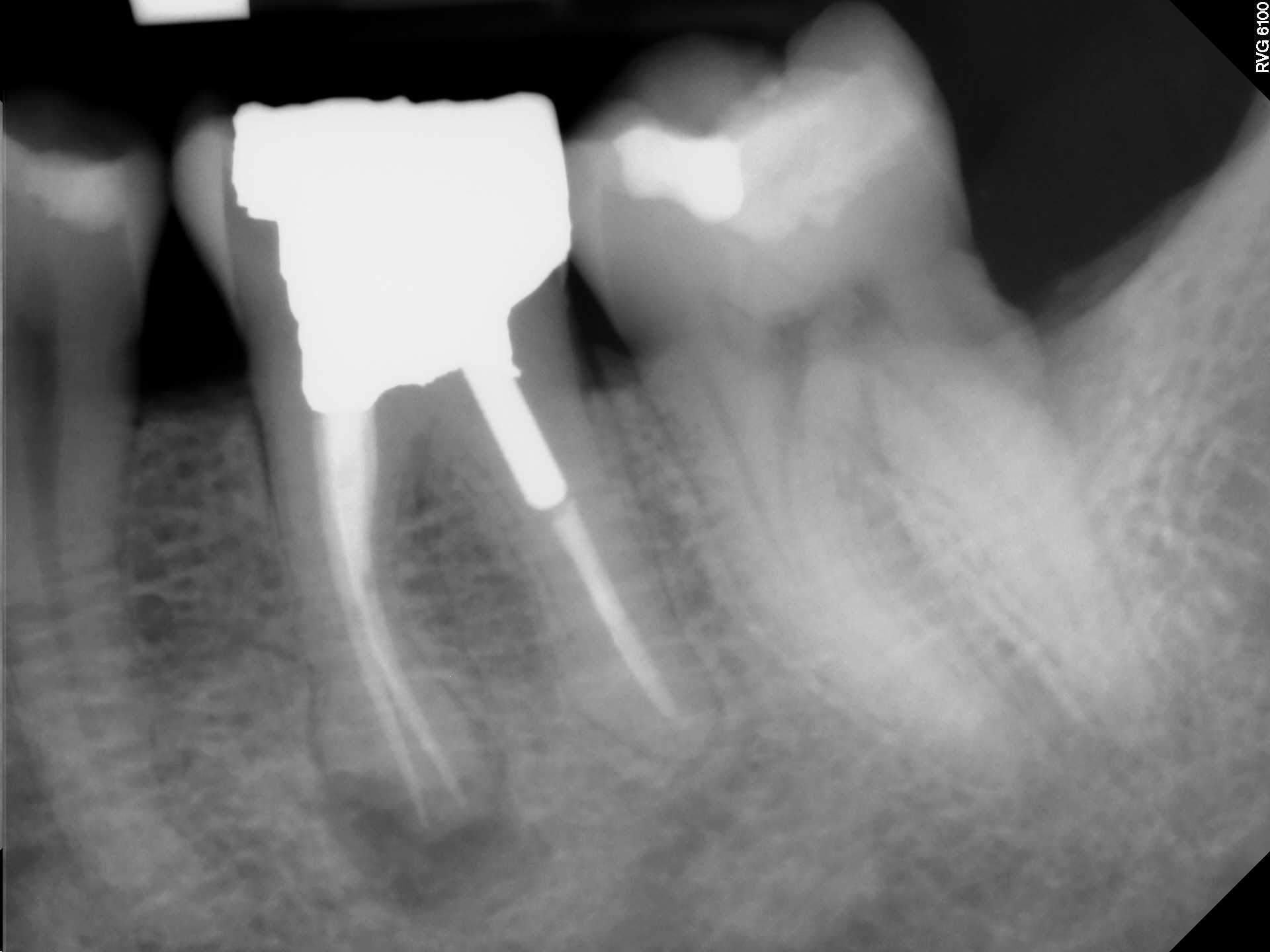
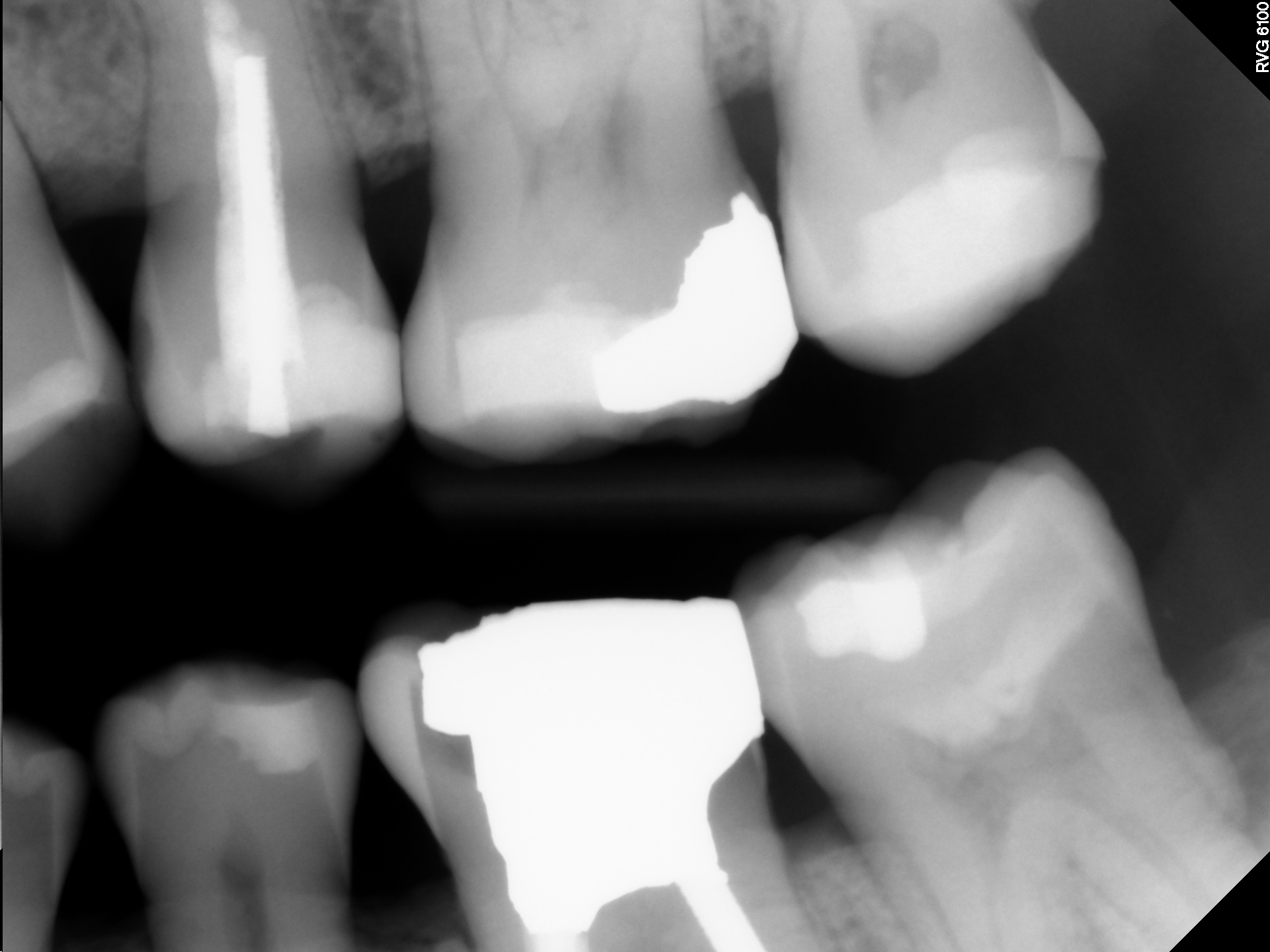

This 48 year old male patient was referred to me by their dentist for consideration of Endodontic treatment of tooth #36. The patient had a history of discomfort that was described as minimal . The pain was localized to the tooth and buccal gingival area and was relieved by Advil. There was no swelling and the patient was relatively asymptomatic on presentation. His referring dentist was concerned about the periapical radiolucent finding at the mesial root apex. The tooth had been restored with an extremely large amalgam/ post/ core . It is my understanding that the buccal cusp fractured off after the Endodontic treatment was completed and that a new core was placed sometime after. The referring dentist was considering restoring the tooth with a full Crown but was concerned regarding the persistence of the radiolucent finding at the Mesial root apex.
Because the patient was asymptomatic on presentation, his motivation level was rather low. I explained that the radiolucent finding at the root apex was of concern to his general dentist and that he could not comfortably place a final restoration on this tooth knowing that the area had not adequately healed. I offered the patient both nonsurgical and surgical treatment alternatives as well as the possibility of extraction and implant replacement in another office. I reiterated that the mesial root was thin and that as more tooth was expended during conventional retreatment, the chance for fracture increased. It was also possible that the tooth may still require surgical retreatment if it did not respond to conventional endodontic retreatment.
This discussion goes to the complicated concepts of “disease versus disease that matters”. In the eyes of patients, asymptomatic disease ( asymptomatic radiolucent findings or minimal symptoms) frequently results in them rejecting further treatment and leaving “well enough alone”. Dentists wishing to restore over such teeth are faced with the prospect of either restoring over teeth that have radiographic signs that these areas have not healed or rejecting the patient’s request for treatment until these issues are addressed as they see fit.
Ultimately, it is the patient’s decision as to whether they wish to proceed. If we choose to place the Crown in this tooth in its current condition, there is a possibility that the tooth would remain completely asymptomatic for the rest of the patient’s life.
Alternatively, should the restoration be placed and THEN the tooth become symptomatic, the option to retreat the tooth conventionally becomes much more complicated because need to access through the crown/post/core complex of the new restoration. That may push us toward a surgical solution.
As long as the patient understands the risks involved and the increased chances that any further retreatment may have to be done surgically, then informed consent has been satisfied and restoration may proceed without retreatment, as they request. It may not be the best solution as we see it, but ultimately it is the patient who must make the choice of whether to treat or not treat what we believe to be a less than optimal situation. In such cases a documented, signed consent to treatment should always be part of the patient’s chart.
