Salvaging a Cracked Molar
This is a 59 year old male patient who came in with a localized complaint of pain for approximately one week. They had been awakened at night and the pain was increasing. The pain was described as 8 out of 10 and radiated from the posterior right mandible anteriorly. The ache was described as radiating and throbbing however he did not have lingering pain. The area was more sensitive to heat than to cold and was increased by pressure and by eating and heat stimulus. Nothing seemed to relieve the pain although the patient did initially have some success with cold water baths and analgesics. There was no swelling in the area . #46 had a large composite (possible MB pulp horn exposure- see BW?). #47 had a very shallow DO composite that was barely through the enamel. But the composite had a crack in it, extending mesially from the distal marginal ridge. Although #46 was more heavily and deeply restored, the pain seemed to be originating in the 2nd molar, #47.

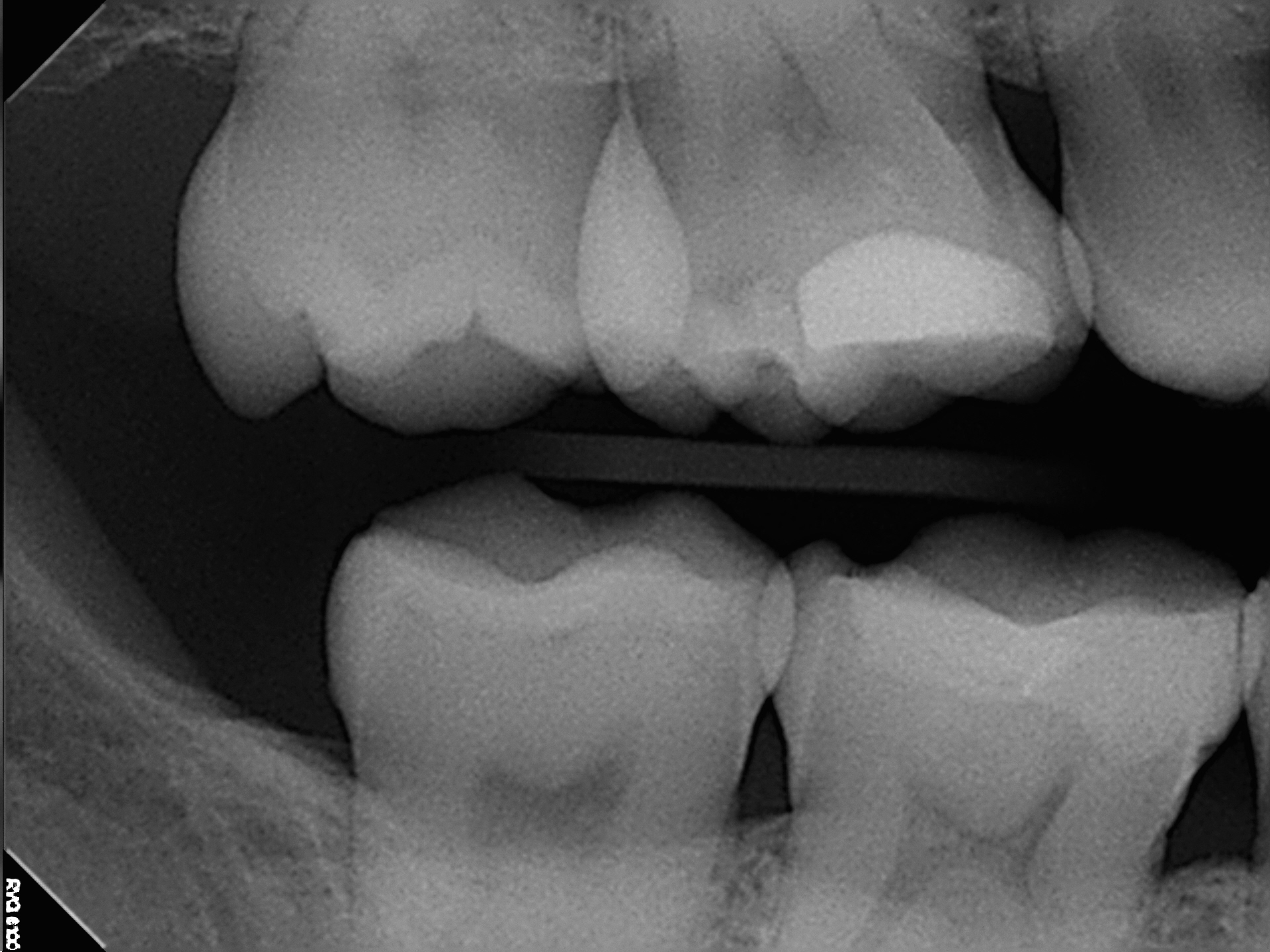
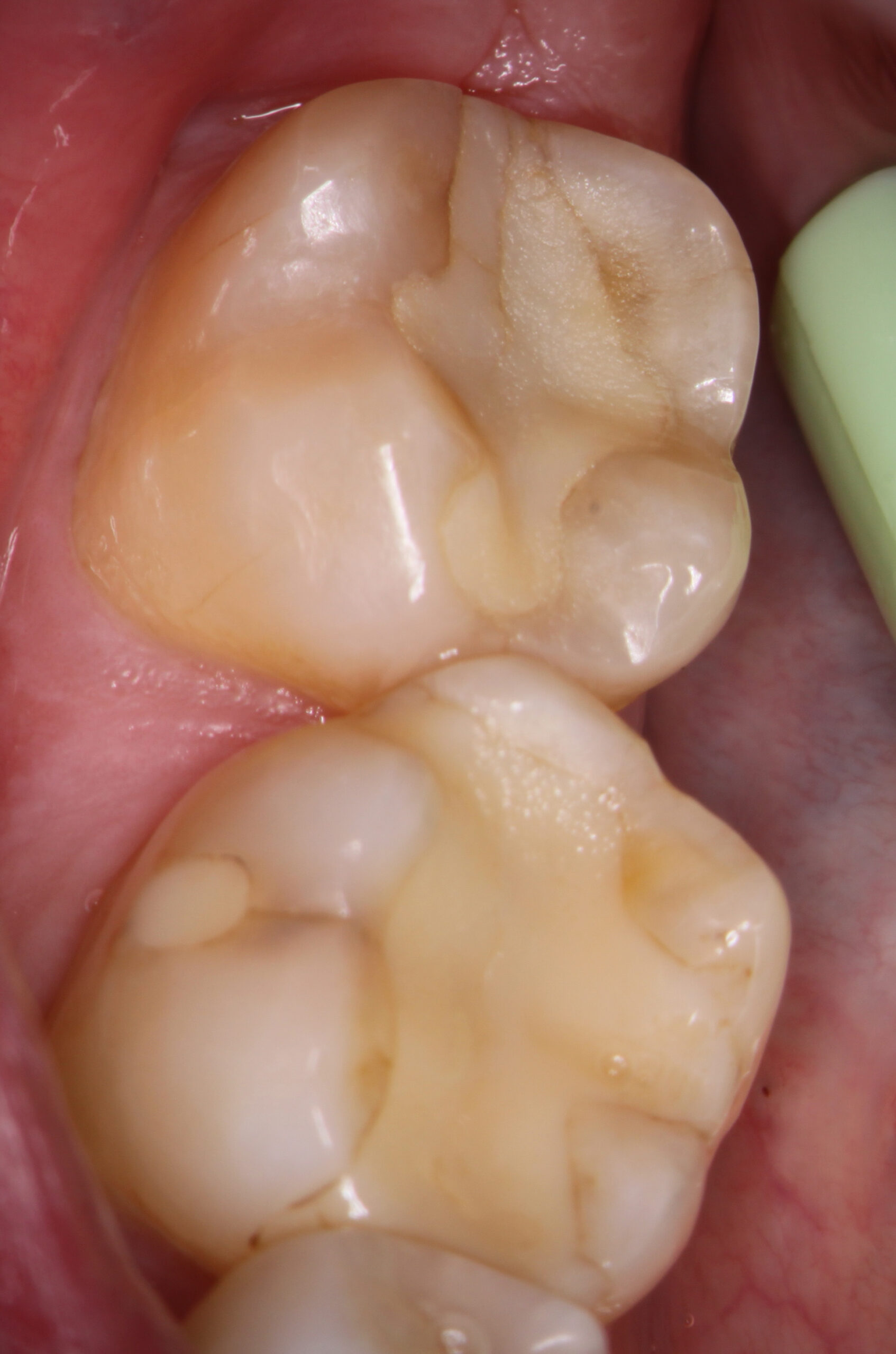
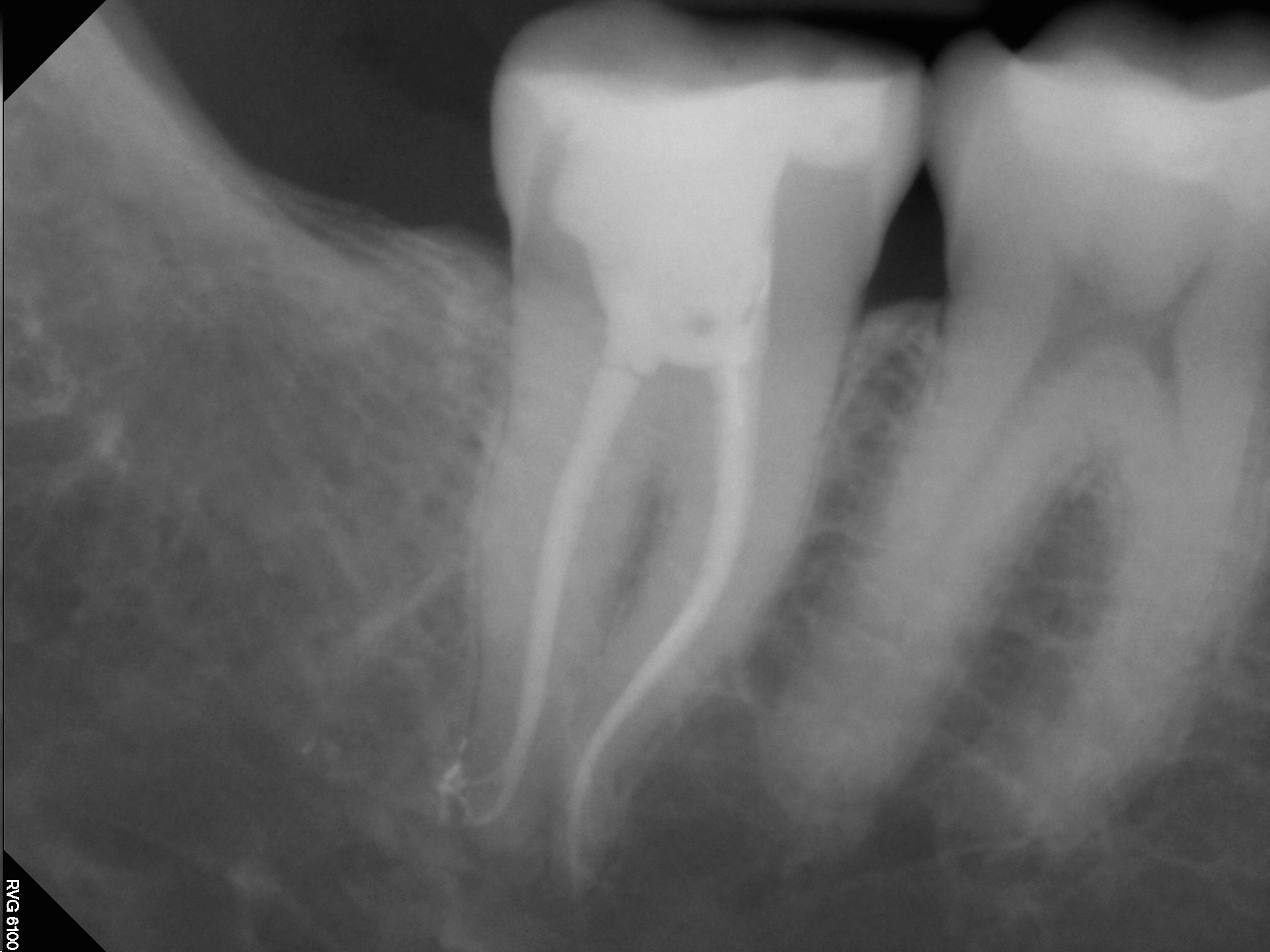
Mandibular second molar teeth have a high rate of mesial-distal fracture, even in Virgin molars. In this case transillumination showed a mesial-distal crack. Pulp tests were negative to thermal stimulus in #47 (positive in #46) and #47 was definitely percussive sensitive. Bitewing radiography showed no associated loss of bone on the proximal surface and periapical radiography showed no evidence of unusual periapical findings (perhaps a bit of thickening at the D root apex of #47?). I felt reasonably comfortable in proceeding with Endodontic treatment on #47 provided that the tooth had full cuspal coverage immediately after treatment.
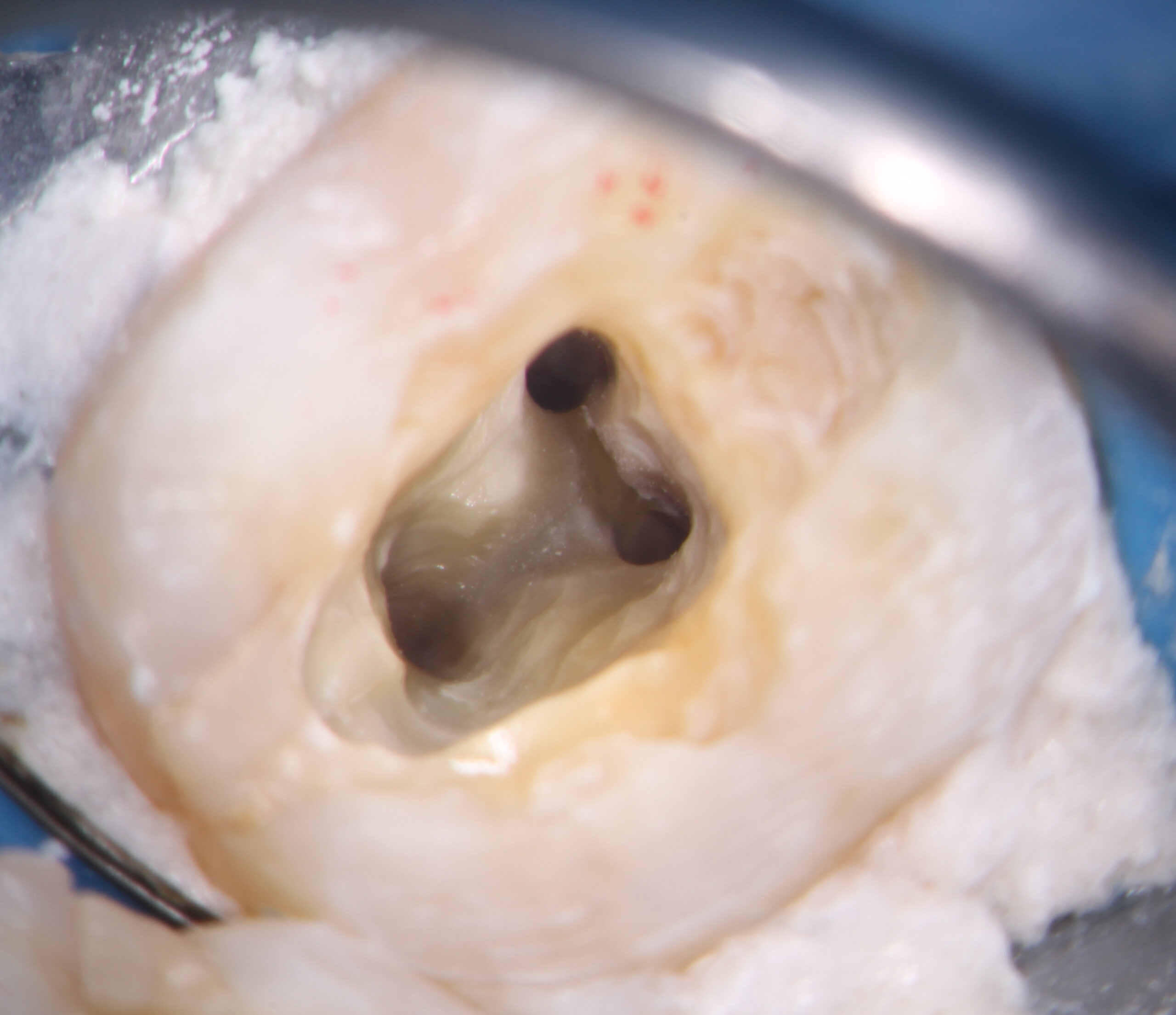
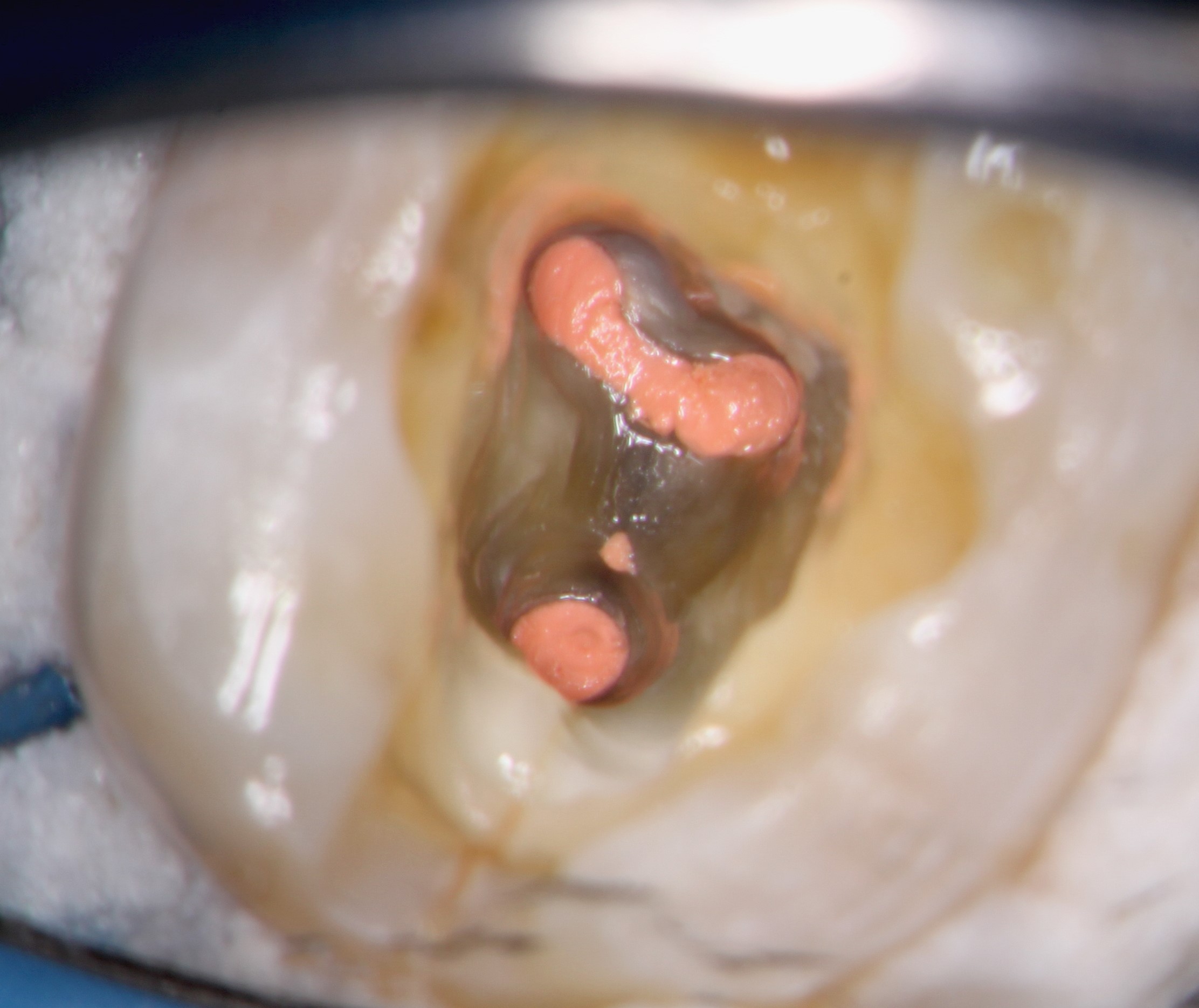
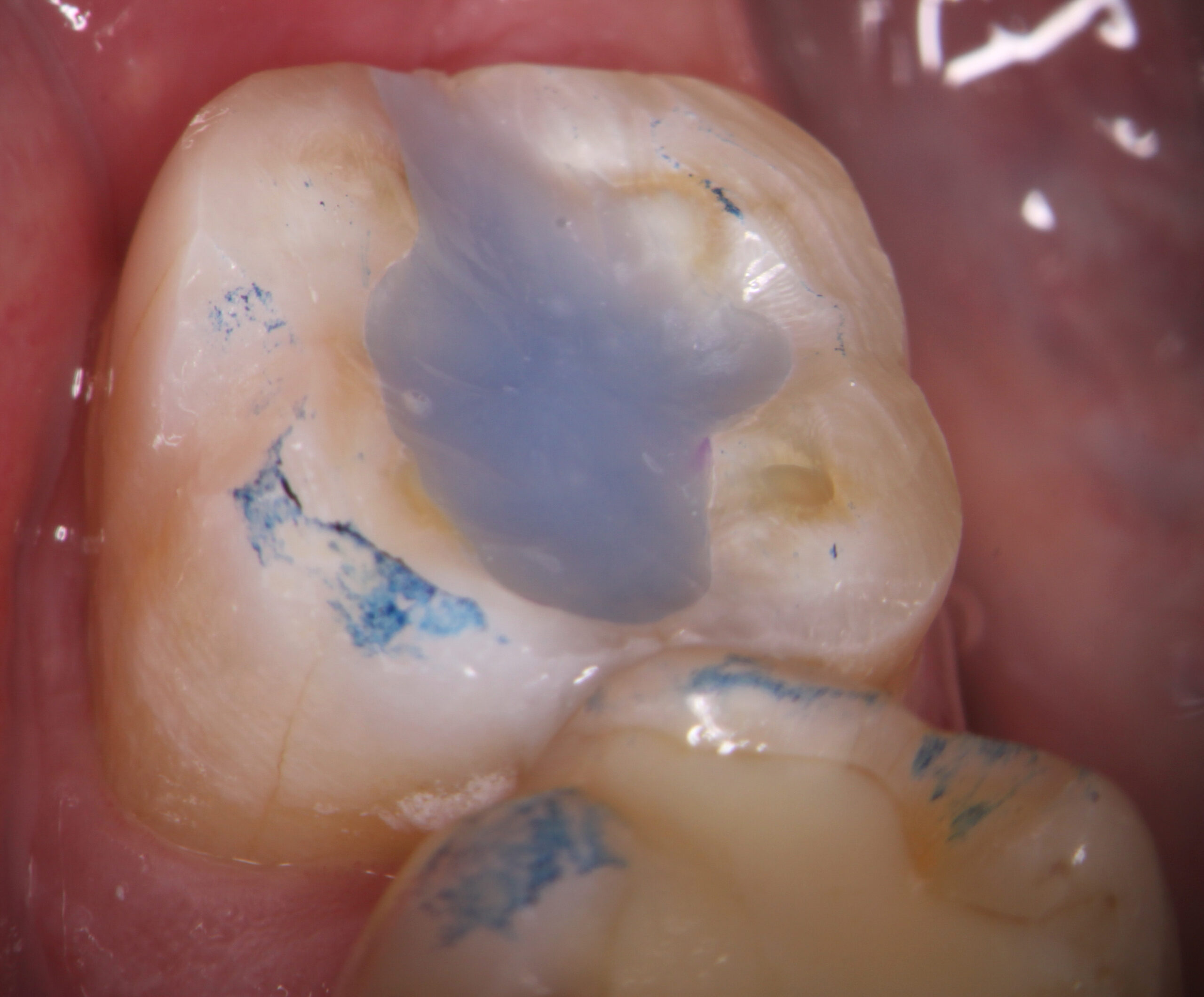
I explained to the patient that but the pulp in #47 had become necrotic due to the fracture and that this had resulted in the acute symptoms he was experiencing. The tooth would require Endo treatment followed by immediate full cuspal coverage restoration. Endodontic treatment was performed without incident (pulp was found to be only partially vital) and was sent back to the referring Dentist for immediate restoration . The patient returned for one year postop recall completely asymptomatic with a nicely restored Crown . The proximal bone appears to be normal and the overall prognosis appears to be good.
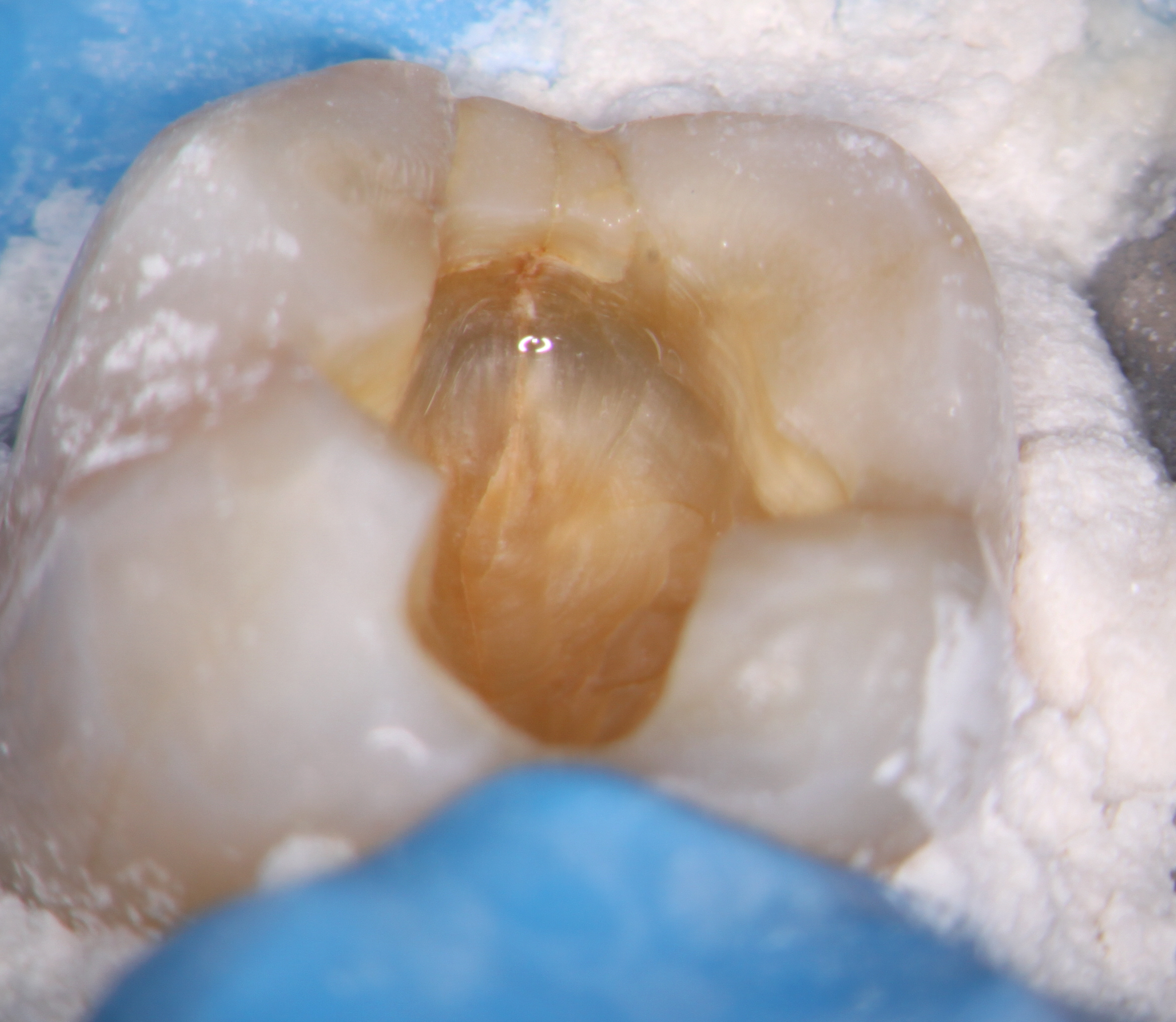
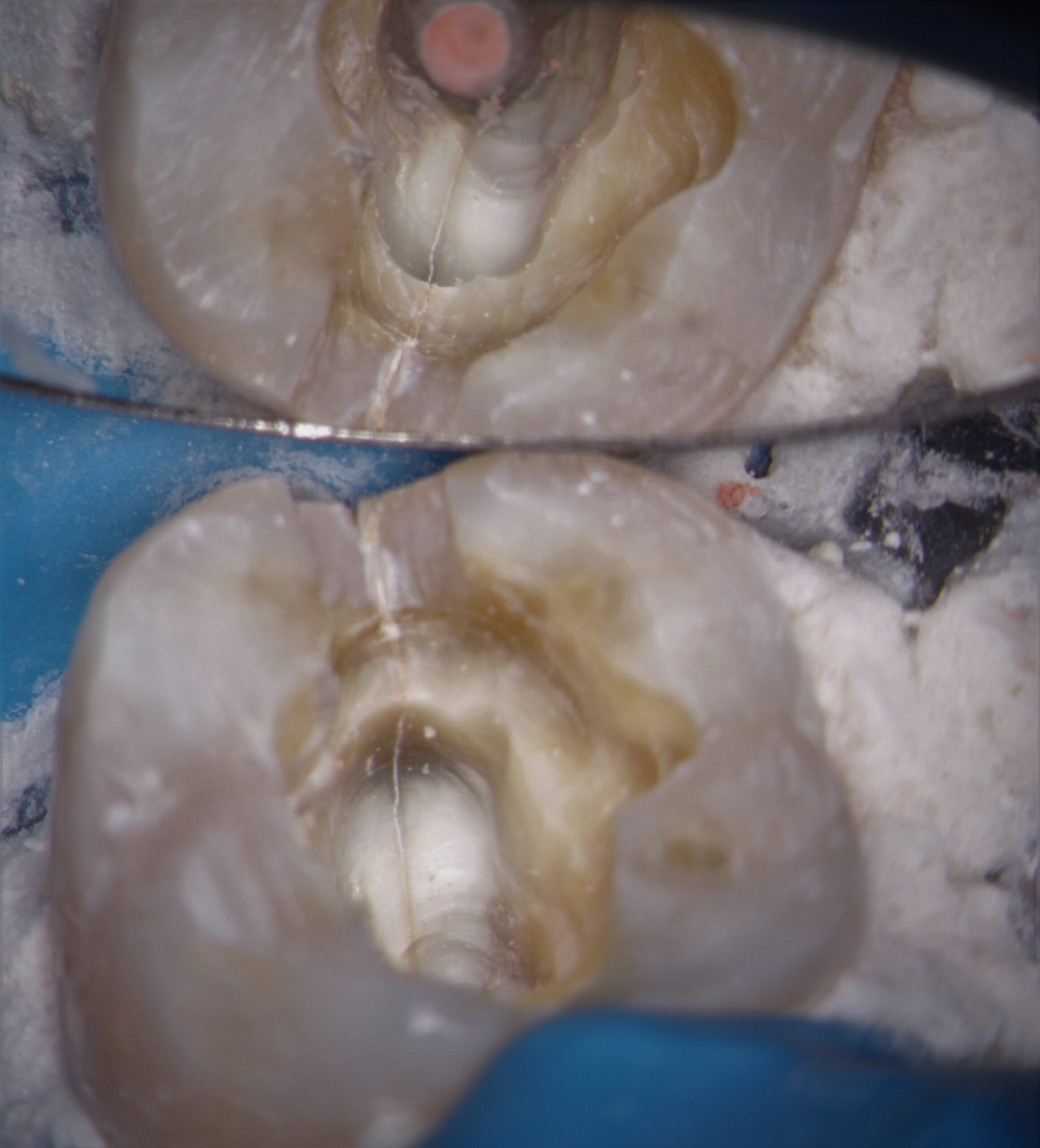

Mandibular second molar teeth have a high rate of mesial-distal fracture, even in Virgin molars. In this case transillumination showed a mesial-distal crack. Pulp tests were negative to thermal stimulus in #47 (positive in #46) and #47 was definitely percussive sensitive. Bitewing radiography showed no associated loss of bone on the proximal surface and periapical radiography showed no evidence of unusual periapical findings (perhaps a bit of thickening at the D root apex of #47?). I felt reasonably comfortable in proceeding with Endodontic treatment on #47 provided that the tooth had full cuspal coverage immediately after treatment.
I explained to the patient that but the pulp in #47 had become necrotic due to the fracture and that this had resulted in the acute symptoms he was experiencing. The tooth would require Endo treatment followed by immediate full cuspal coverage restoration. Endodontic treatment was performed without incident (pulp was found to be only partially vital) and was sent back to the referring Dentist for immediate restoration . The patient returned for one year postop recall completely asymptomatic with a nicely restored Crown . The proximal bone appears to be normal and the overall prognosis appears to be good.


Over my 35+ year Endodontic career I have transitioned somewhat in my decisions to treat or not treat such cases. The first thing I look for is the opposing tooth, which often is it full Crown restoration. Teeth opposing crowns are frequently associated with higher rates of fracture in restored or even Virgin opposing teeth.
There are two factors that determine whether I recommend that patients proceed with Endodontic treatment and restoration:
#1. If the pulp is testing non-vital and there are periapical areas in the furcation and at the apices, there is a VERY good chance that the crack is extensive. If the crack is either close to the furca or traverses it completely. (This can only be confirmed with crack visualization) I believe that the tooth is a poor candidate for rehabilitation.
#2. The depth of the pocketing along the fracture line. If the pocketing is greater than 6 or 7 millimeters, and there is associated vertical bone loss, again the tooth is deemed to be a poor candidate for treatment and I recommend extraction.
There will always be patients who will attempt to salvage teeth like this rather than replacing them with an implant (mostly for financial/insurance reasons) . In those cases I tell patients that it is impossible to determine how long this tooth will last and that somewhere between 2 to 10 years is not uncommon. Retention of these teeth depends on many factors such as response to function, time to final restoration and occlusal factors, many of which cannot be predicted.
