Calcified Maxillary Lateral Proves to be a Challenge
Like the song says, sometimes you gotta “Know when to hold ’em and know when to fold ’em.”
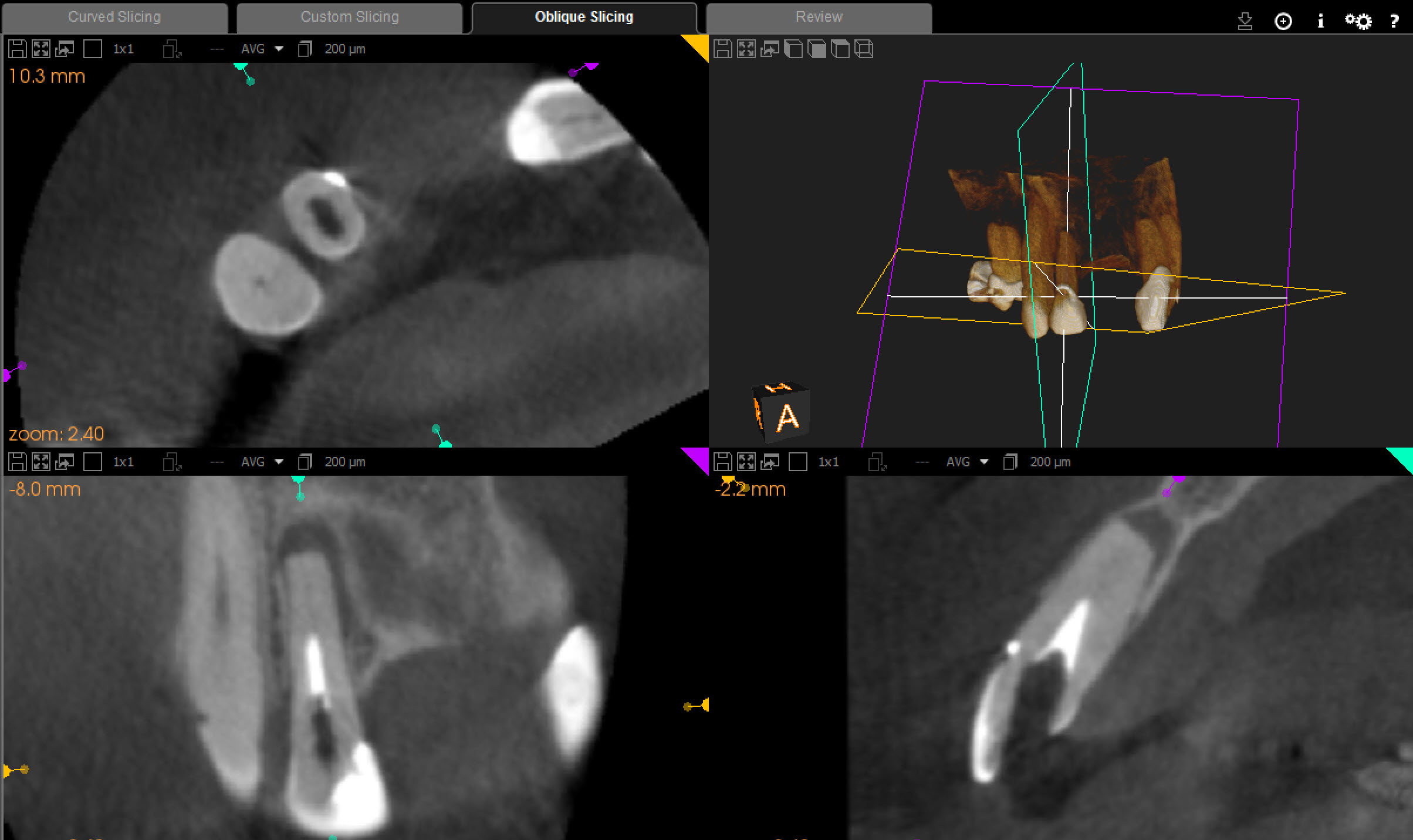
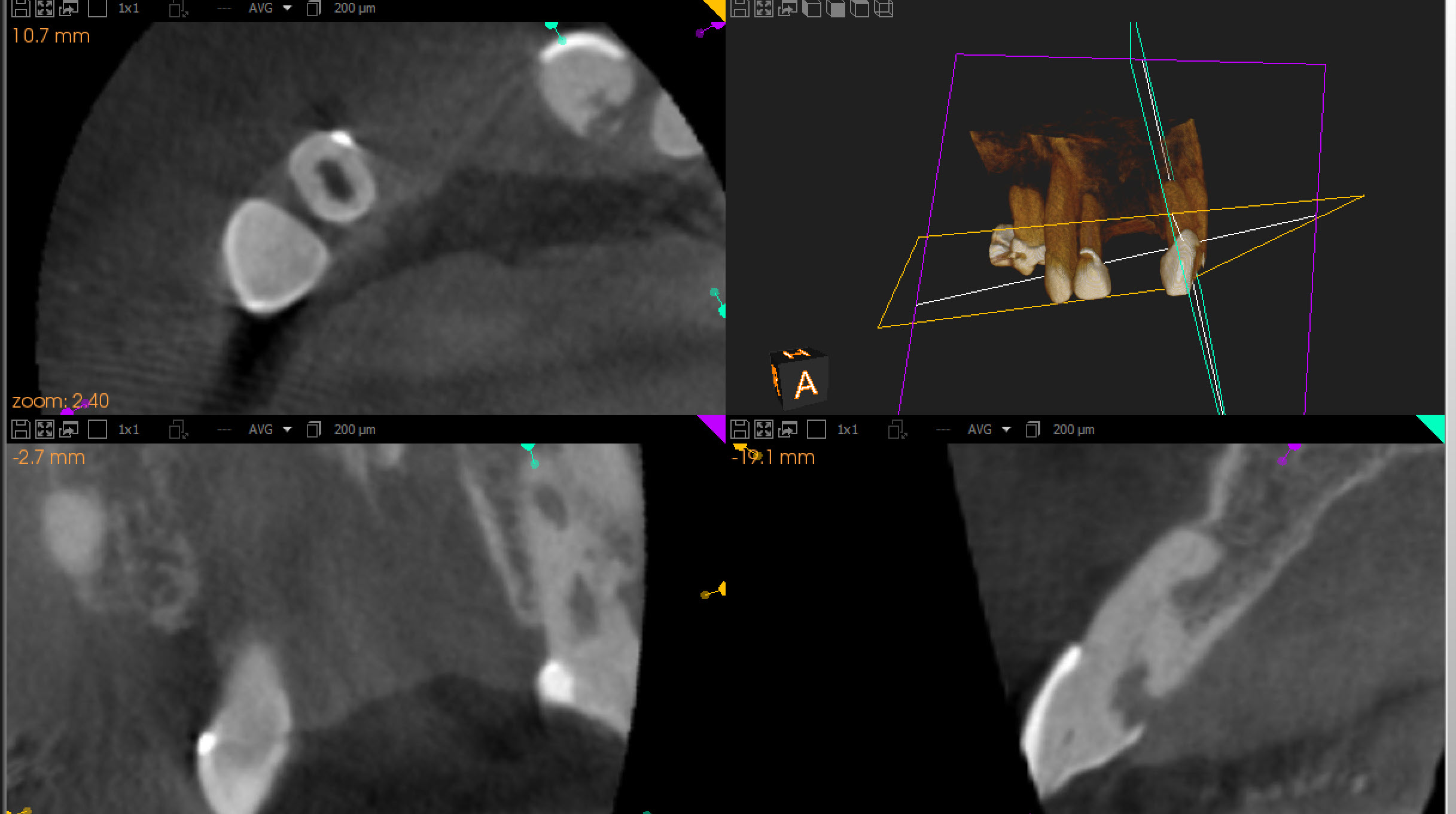
The patient was referred for Endodontic treatment of this Maxillary lateral incisor that had a radiolucent finding at the apex . The patient had been involved in a motor vehicle accident some years ago had lost several teeth during the trauma. The referring dentist had attempted access but could not locate a canal. Wisely, he stopped before hogging out the root or perforating the case and referred the case to me. The canal appeared to be totally calcified on a conventional film with the exception of the apical 2 or 3 mm.

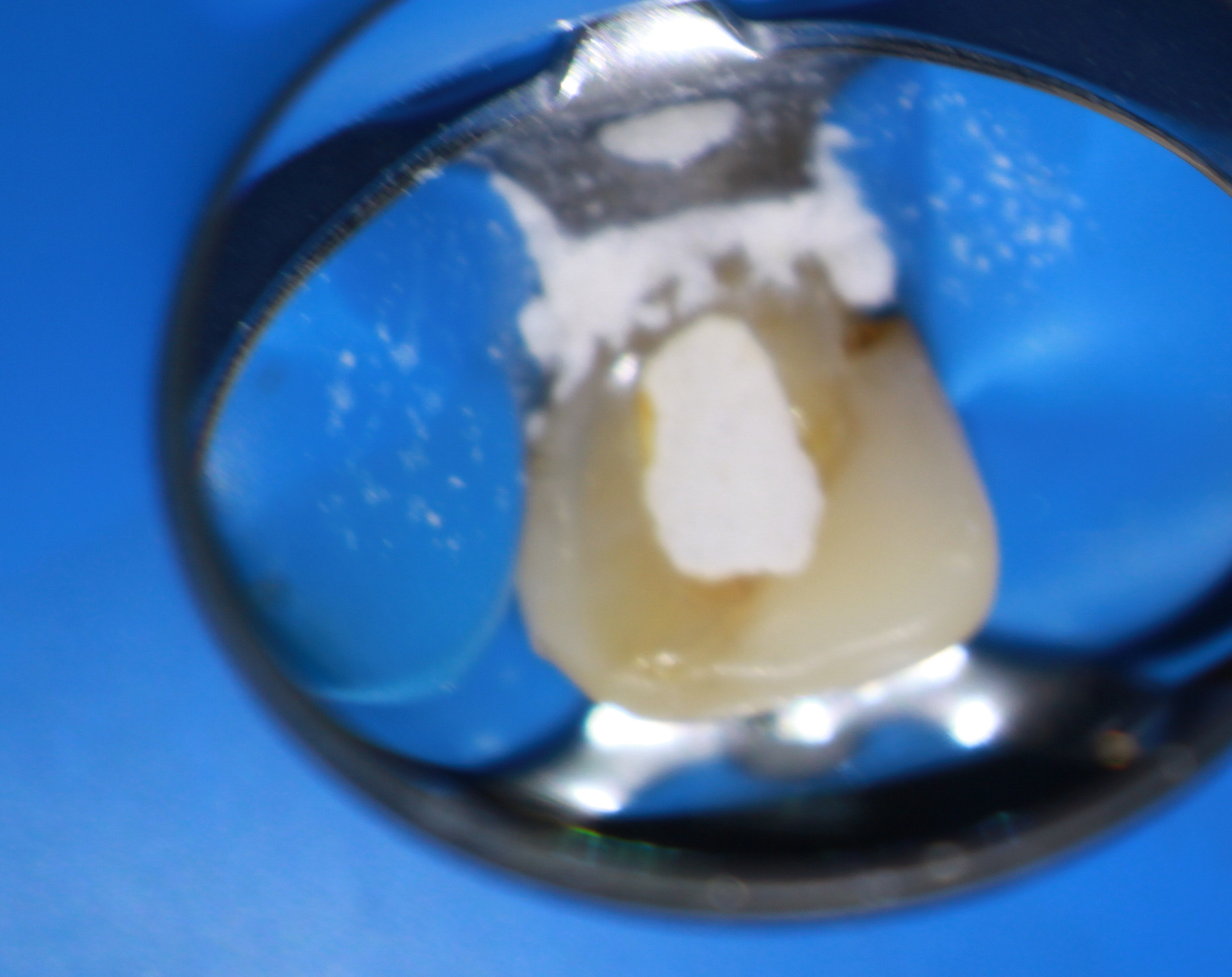
Cone beam tomography also showed that there was little if any canal space except at the apical few millimeters. Nevertheless, we attempted to make Endodontic access into the tooth because we assumed that we would find our way to the apex to deal with this necrotic apical tissue.
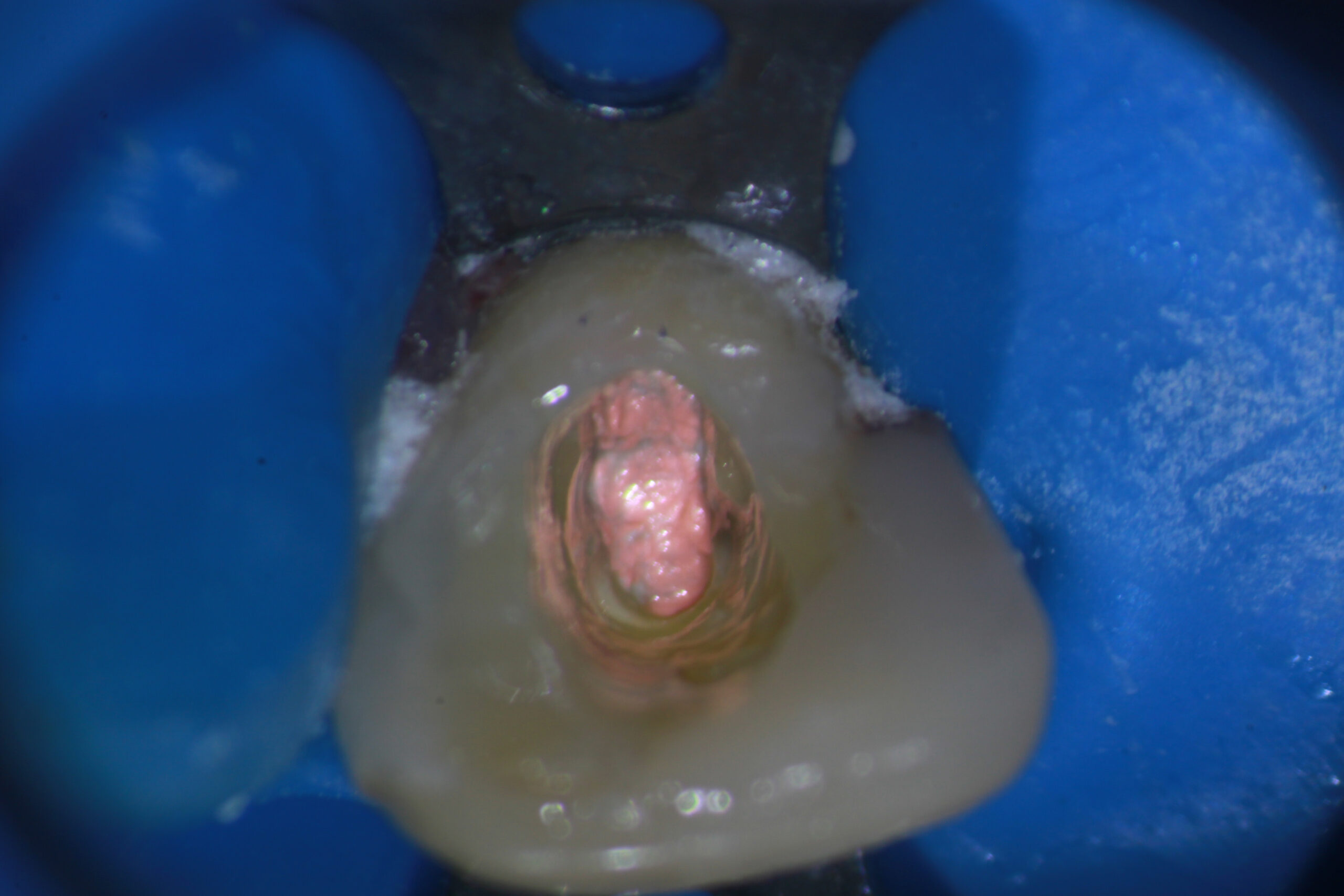
Unfortunately, after going very far into the tooth without being able to find the canal, I realized that further exploration of the tooth could be catastrophic. I was already at the limits of my longest Endo explorer and visibility was becoming an issue (even with a Surgical Operating Microscope and its strong light!) because the access was so small. Control of ultrasonic instruments and Munce Burs at that depth becomes critical in such narrow roots. Continuation would only result in loss of further Dentin, potentially weakening the tooth and risking perforation.
The patient was asymptomatic and we agreed to terminate the treatment at this point by obturating to the most apical extent possible and then sealing the access. If further treatment would be required, it would need to be performed surgically and efforts would need to be made to try to preserve as much of the root as possible, should that be necessary.



The question remains: How do you decide when to “Go To Surgery First” vs. attempting this type of treatment?
In most cases there IS a canal there, albeit very small. Endodontists frequently treat such cases, but there are some where, in hindsight, an initial surgical approach may have been a better option. As with ANY case involving surgery, Periodontal condition, Age and health of the patient, medications such as Bisphosphonates, Hygiene, attitudes toward surgical procedures, presence of an existing RPD that can be added to, how strategic the tooth is to the overall treatment plan Etc Etc ….all play a role in deciding whether a surgery may be a better option.
