What have we learned from this retreatment failure?
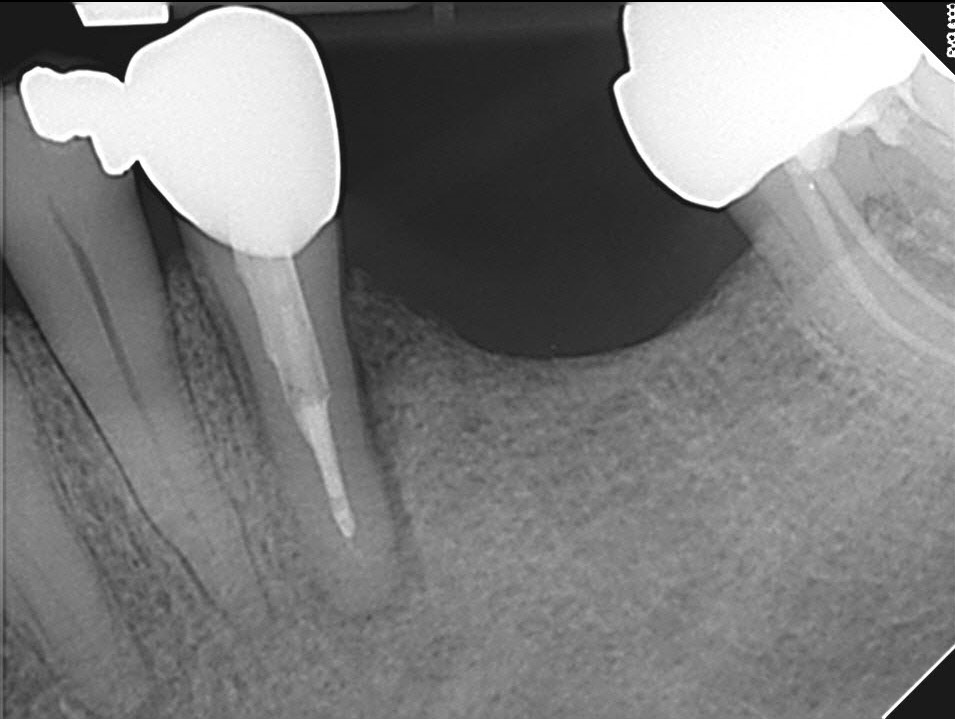
A 61-year-old male was referred for endodontic consideration of #35. The patient had #36 extracted by his dentist two weeks previously. Reason unknown. A Bridge is planned for #35-37. The referring dentist noted a radiolucent area associated with the apex of #35. Percussion, Palpation, chewing, and Periodontal findings were all within the range of normal in #35. #37 was unopposed. The endodontic treatment in #35 appeared short filled and radiography confirmed the presence of a large stainless steel post and diffuse radiolucency at the apex of the root. Clinical examination revealed an open buccal margin associated with the crown of #35. I was unsure of whether coronal leakage may be playing a factor in the Endo failure. However, the patient was asymptomatic at the time of examination.
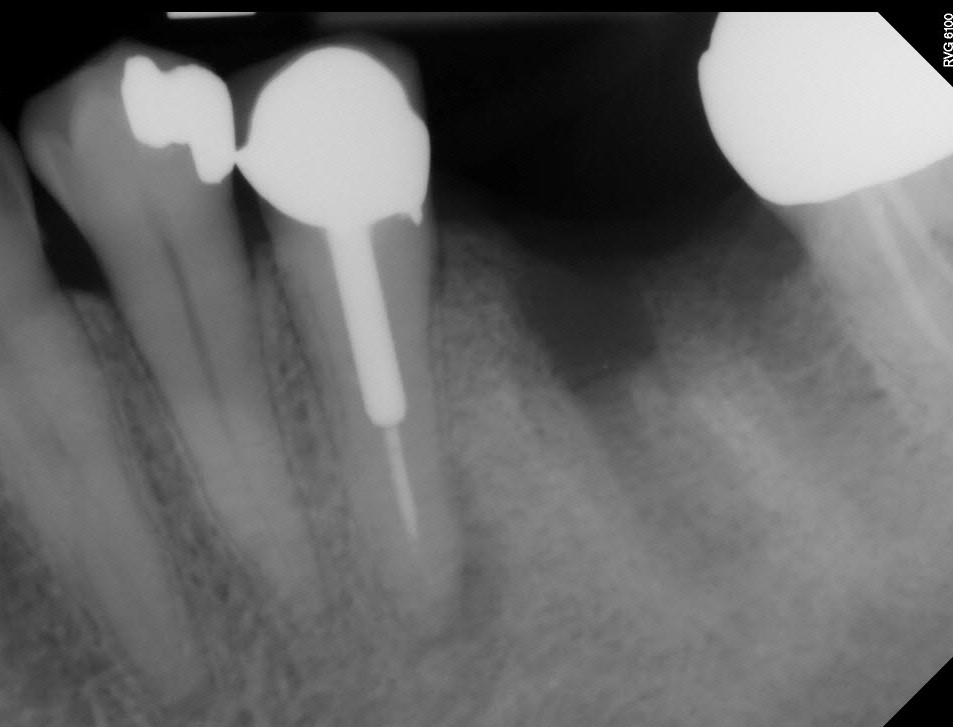


Although we were considering conventional disassembly retreatment to address the persistent periradicular findings, I was very concerned that the tooth would not survive post removal attempts. Even if we did remove the post, I did not believe the remaining root would serve as a good abutment because of its compromised dentin thickness.
I spoke with the Dentist and suggested that he could simply remake the existing single crown and place an implant in the position of #36. Placing a new crown over asymptomatic #35 (WITHOUT retreatment) meant that the patient would have to sign off on placing a new crown over than a less than optimal Endo treatment and apical pathology. However, disassembly retreatment may leave the tooth in a poorer condition without guaranteeing resolution of the apical radiolucency. Should #35 become symptomatic in the future, we could disassemble it, treat it surgically or extract it and restore the area with two implants (#35 and 36), rather than trying to merely replace the crown in #35.
Two years later, the patient was again referred to me for further examination. The crown had been replaced over the existing post and core. The RD noted that the radiolucent area was now larger, but the patient remained asymptomatic. I explained to the patient that we again had several options:
1. Disassembly retreatment and re-restoration
2. Surgical treatment or
3. No treatment until symptomatic.
4. Extraction and implant replacement.
Since he had only recently had the crown replaced and was asymptomatic, the patient again chose not to retreat the Endo.


One year later the patient began to have symptoms. For the previous 2 weeks he had been having difficulty chewing and now wished to address the problem. The RD informed me that he was planning to use #35 as an abutment for bridge or RPD. He and the patient agreed to disassembly retreat.
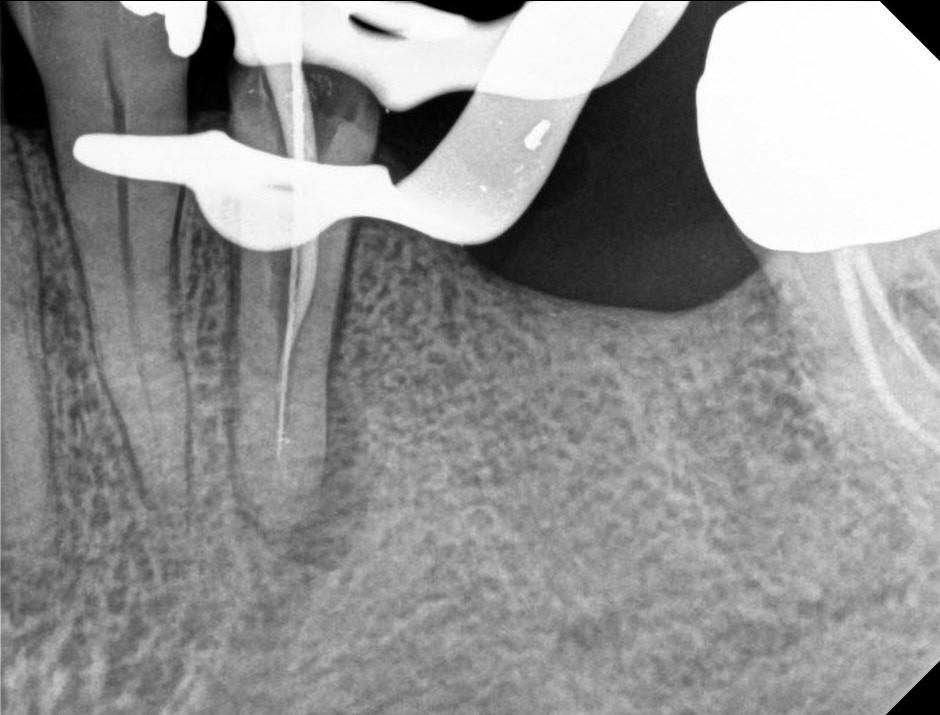
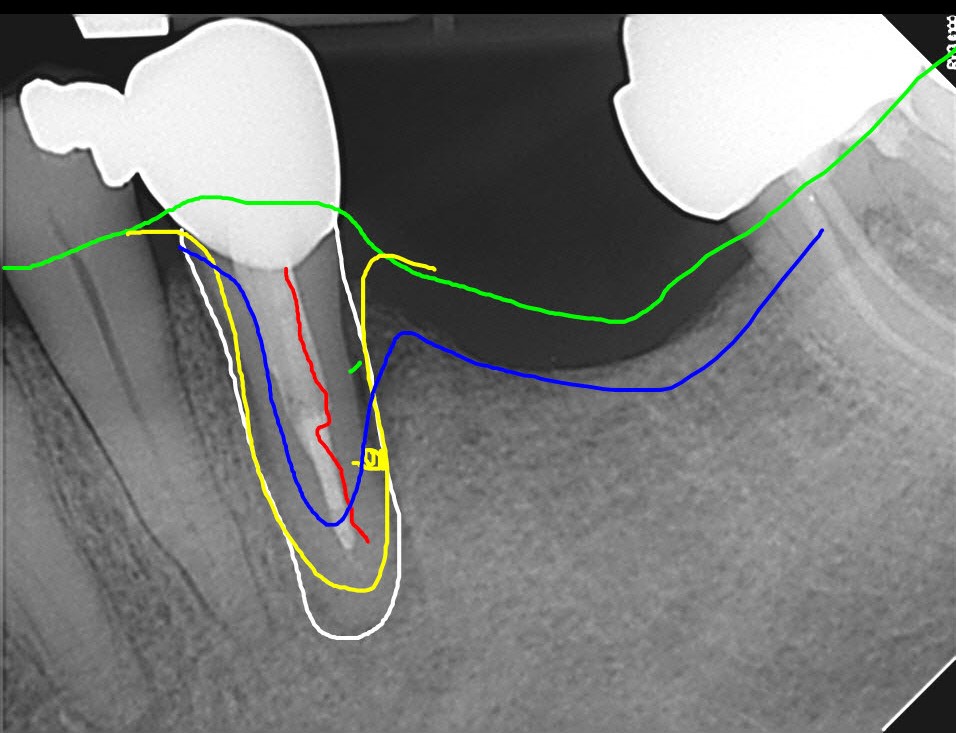
Retreatment was initiated with removal of the crown, post, attempted re-clean of the canal and Ca(OH)2 medication. (The Gutta Percha cone I placed into the canal along side the WL file in the image below was used only to help prevent the loose file from falling out when taking the WL image). The canal was found to be blocked short of the terminus.

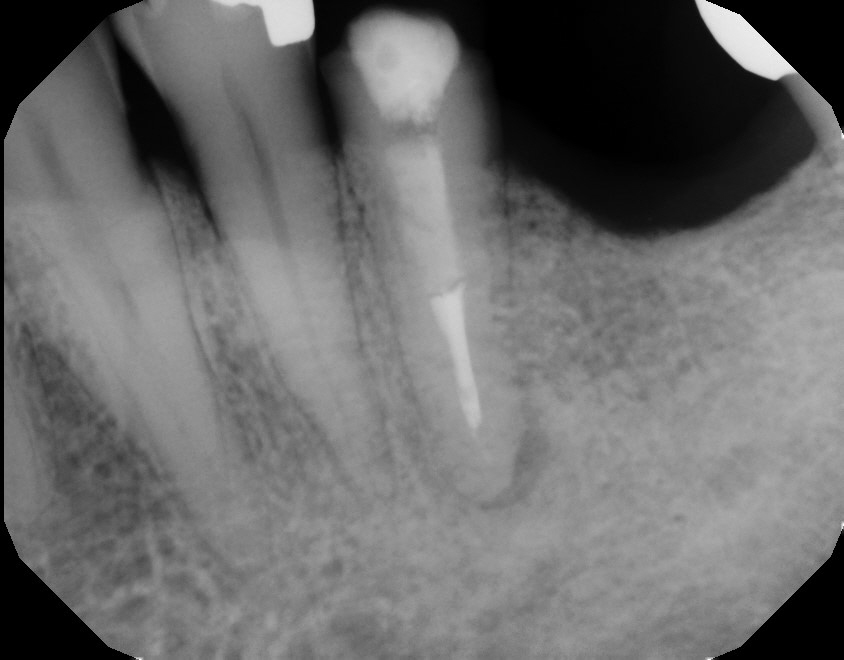
After 1 month of Ca(OH)2 medication the area was asymptomatic and the canal obturated. A post space was left for the RD with instructions NOT to modify it. The patient did not appear for his scheduled 4 month follow up.



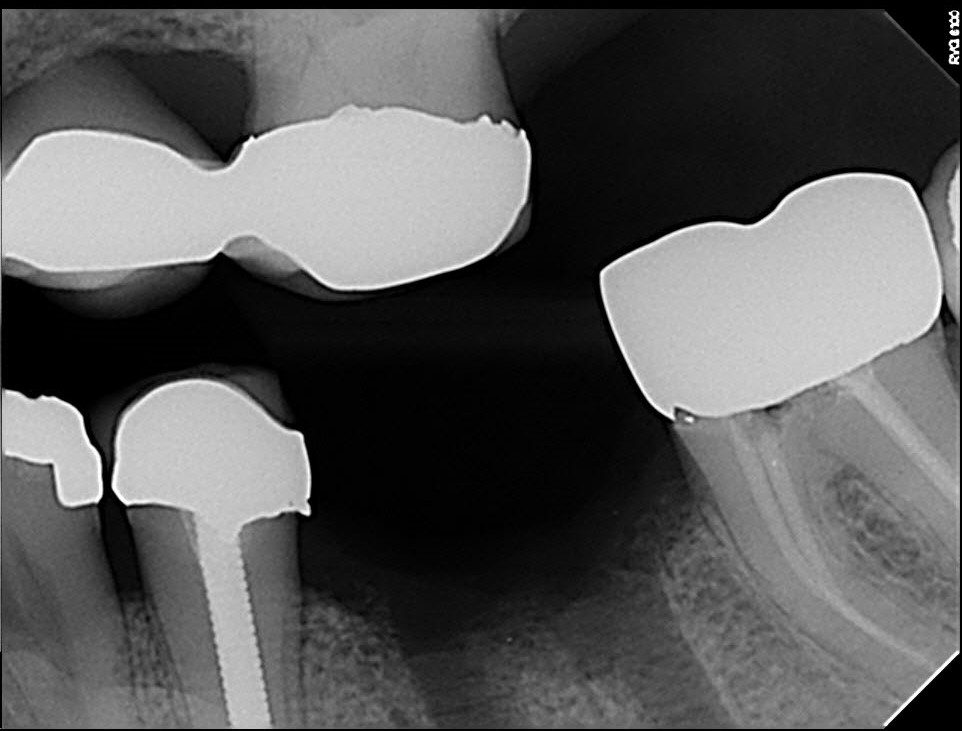
A 6 mo. postop radiograph was sent to me by RD that showed l improvement in the apical radiolucency. Although the area had not completely resolved, it appeared that retreatment results were moving in the right direction, and I recommended that the RD proceed with the final restoration.
Two and a half years later, the patient called to schedule an appointment for recall of tooth #35. The patient reported that the tooth has become very sore. He had avoided chewing on the left side and has developed a “pimple” on the side of the tooth.
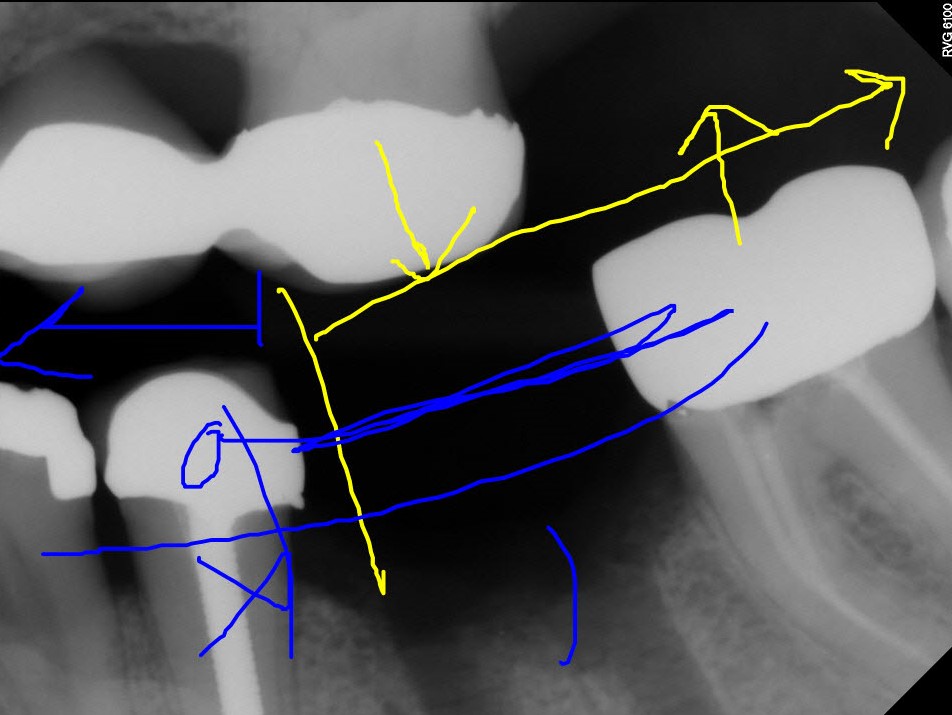
Clinical examination revealed a draining buccal sinus and 10-millimeter probing depth on the buccal aspect of the root. Radiographic examination showed good healing of the apical radiolucency but PDL thickening was noted on the distal aspect of the root along with some vertical bone loss. This is generally consistent with the presence of a root fracture.

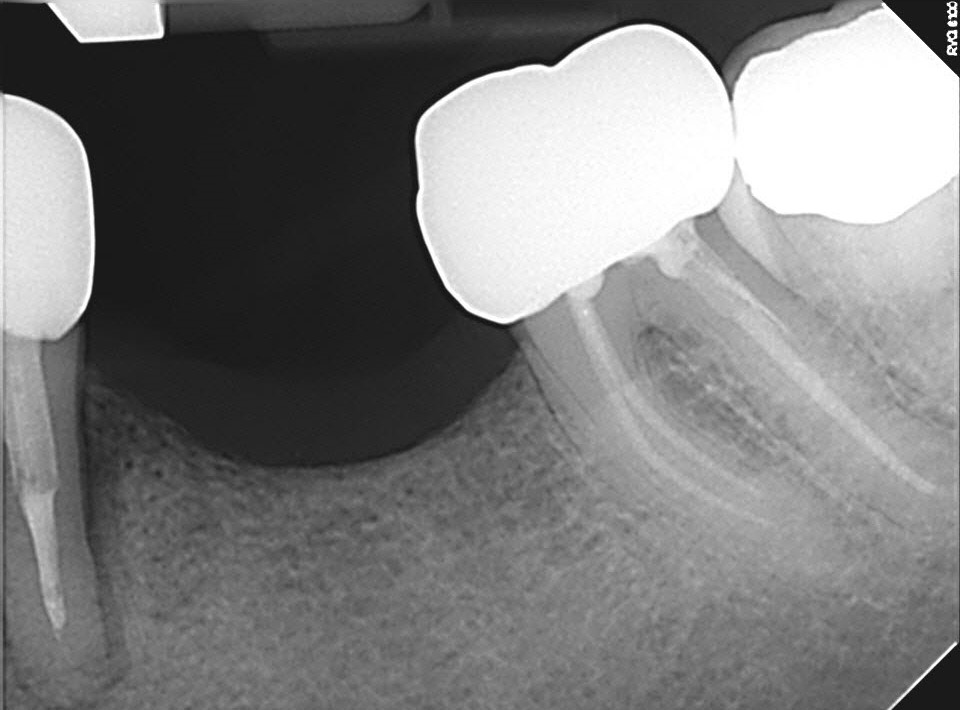
I told the referring dentist that #35 required extraction. The apical area had actually healed quite well but I believed that after completion of the retreatment, it was imperative that #35 NOT be the sole functioning posterior tooth on this side after retreatment, if it were to survive. Without occlusion on # 26 and # 37 this premolar was at high risk of root fracture. The patient now faced the prospect of two implants, a larger bridge or RPD to replace the now missing #35 and 36.
From this case we can see that if if long term retention of the retreated tooth is the goal, Endo retreatment cases must be part of with a well thought out treatment plan that takes into consideration things like prompt post-treatment restoration , occlusion, and function. Even the best Endo will fail if it is not followed up with the correctly designed and implemented restorative treatment.