Surgical Endo Failure Due to Unusual Root Fracture
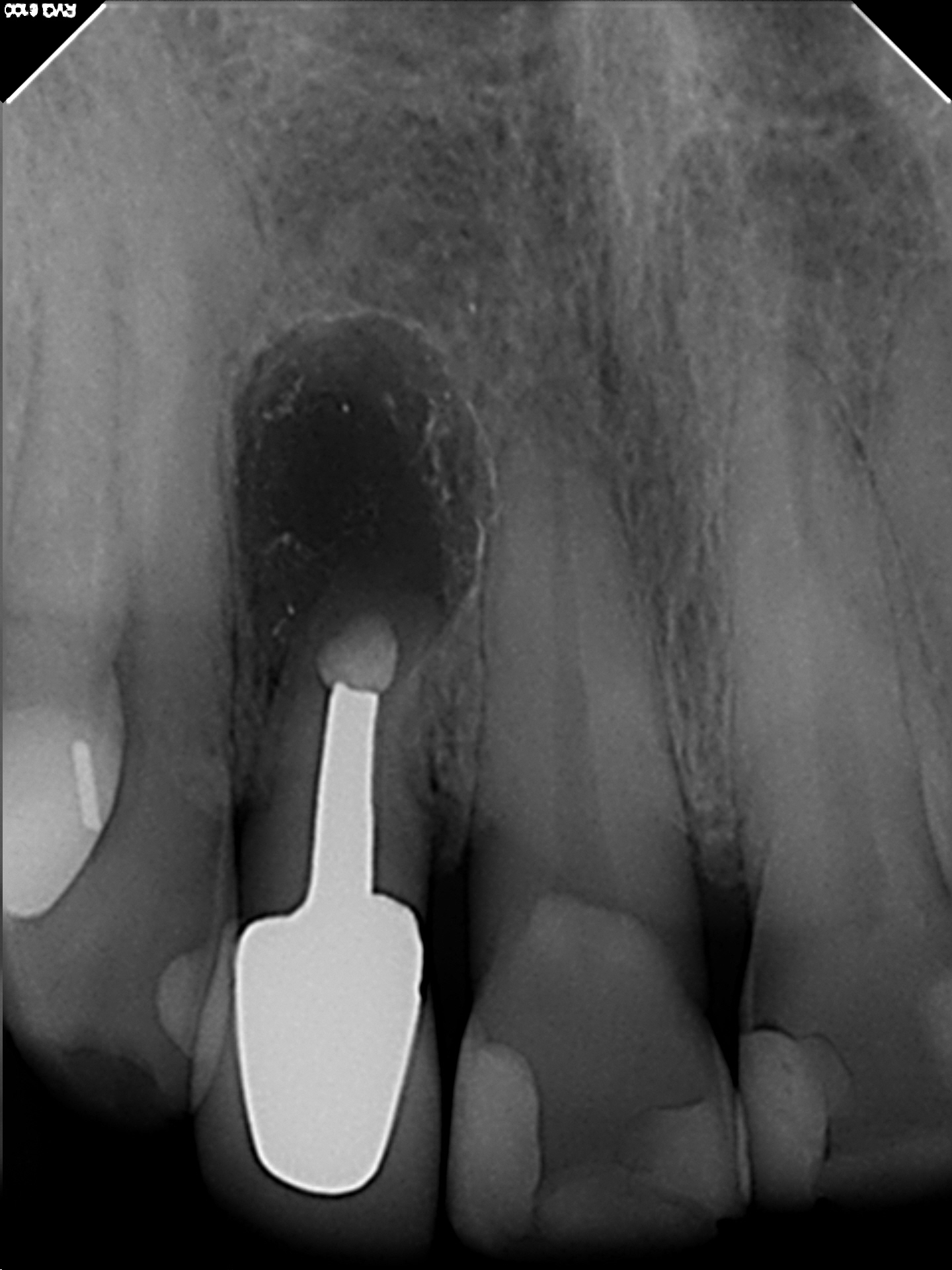
A 55 year old female patient was referred to me in late 2013 for consultation and possible treatment of tooth# 12. The patient had a history of endodontic treatment with post and core crown restoration. The tooth had subsequently been retreated surgically with root resection and Retrofilling. . The crown root ratio was noted to be extremely low and there was a persistent periradicular radiolucent finding associated with the apex of this tooth. A draining buccal sinus was present. I noted that the retro filling material was amalgam, which likely indicated that this surgical treatment was quite old. Furthermore, minimal filling material was noted in the canal, with a void was present between the post and canal filling material.


Clinical examination revealed slight percussive and palpation sensitivity over the apex of# 12. Periodontal probings were within the range of normal. Occlusion showed no extreme function but I was concerned regarding the crown/root ratio and the stresses that might occur should we choose to further resect the already short root There also was the issue of the metal post. Retro-preparing against a metal post cannot be done with the normal ultrasonic surgical instruments and must be done with a carbide bur. This often means further angular resection of the root to allow for surgical handpiece access in a root that was already of minimal length. Further postop stresses on the root could result in eventual fracture considering both its size and minimal root length. I was unsure of the long term prognosis.
After explaining all the options to the patient which included extraction and implant placement or bridge, the patient chose to have the area re-surgerized because she was happy with the current aesthetics of the existing crown.
Unlike the previous surgery (that resulted in scarring of the soft tissue because the incision was made in the mucosa) a classic BU flap was laid in the attached gingiva, coronal to the previous surgical incision.

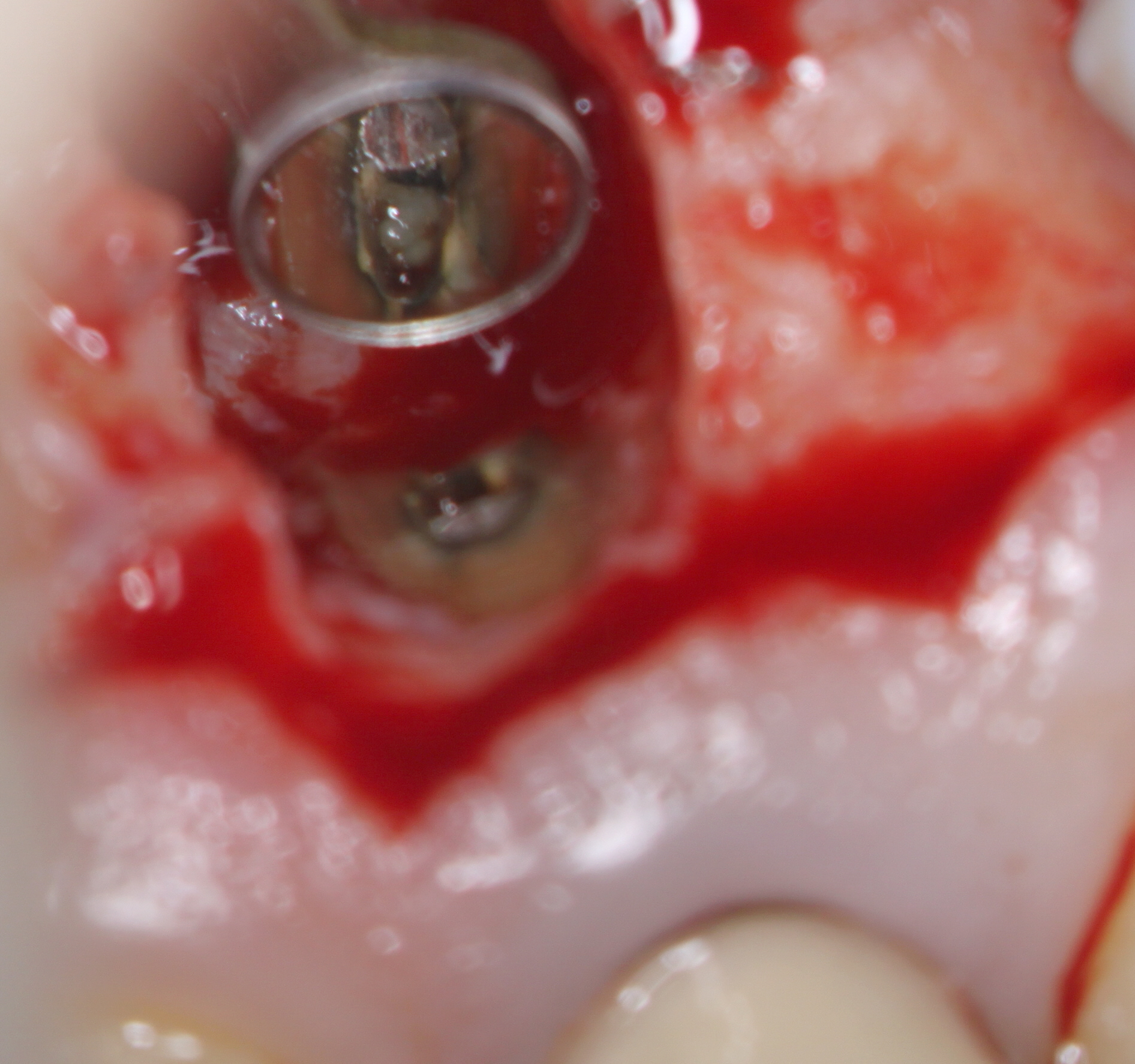
Exposure of the crypt revealed granulomatous soft tissue ingrowth into the resorbed area at the end of the root. and irregular stained root dentin present at the root end. Insufficient tissue was available for biopsy because of its granulomatous nature. I removed only the irregular discolored area of the root resorption. The amalgam was removed and the peripheral canal area around the post root retroprepared as well as possible with ultrasonic retro tips . A small round bur was then used to remove as much of the post as possible (with the restricted access) to allow for placement of a retro filling.
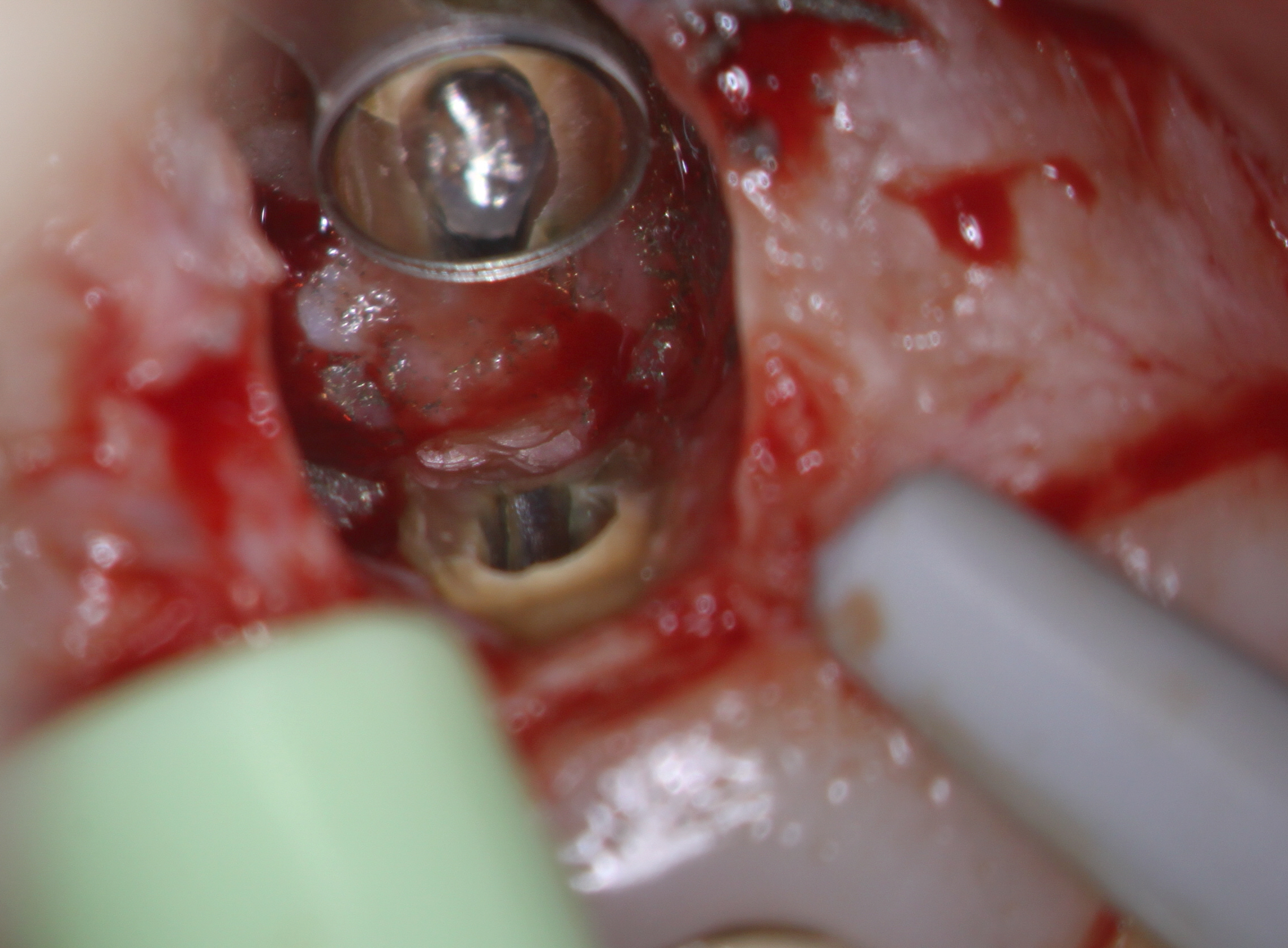
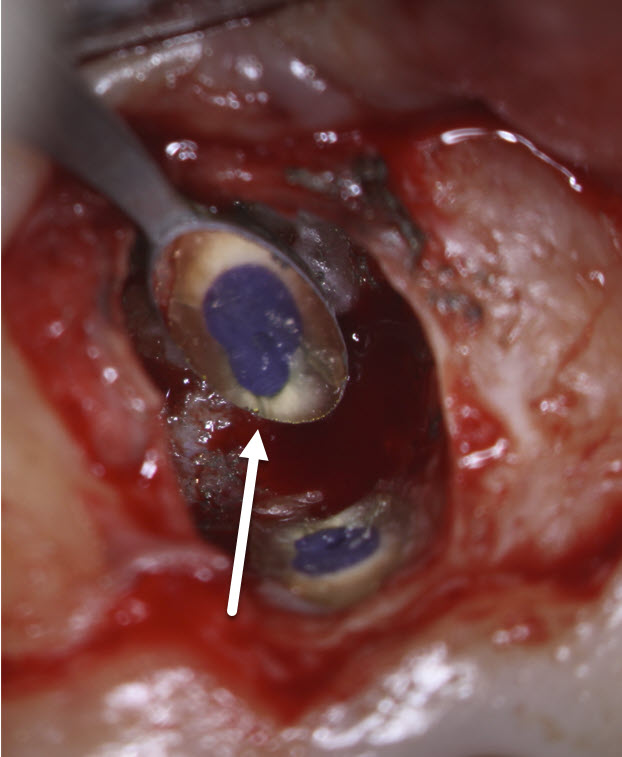
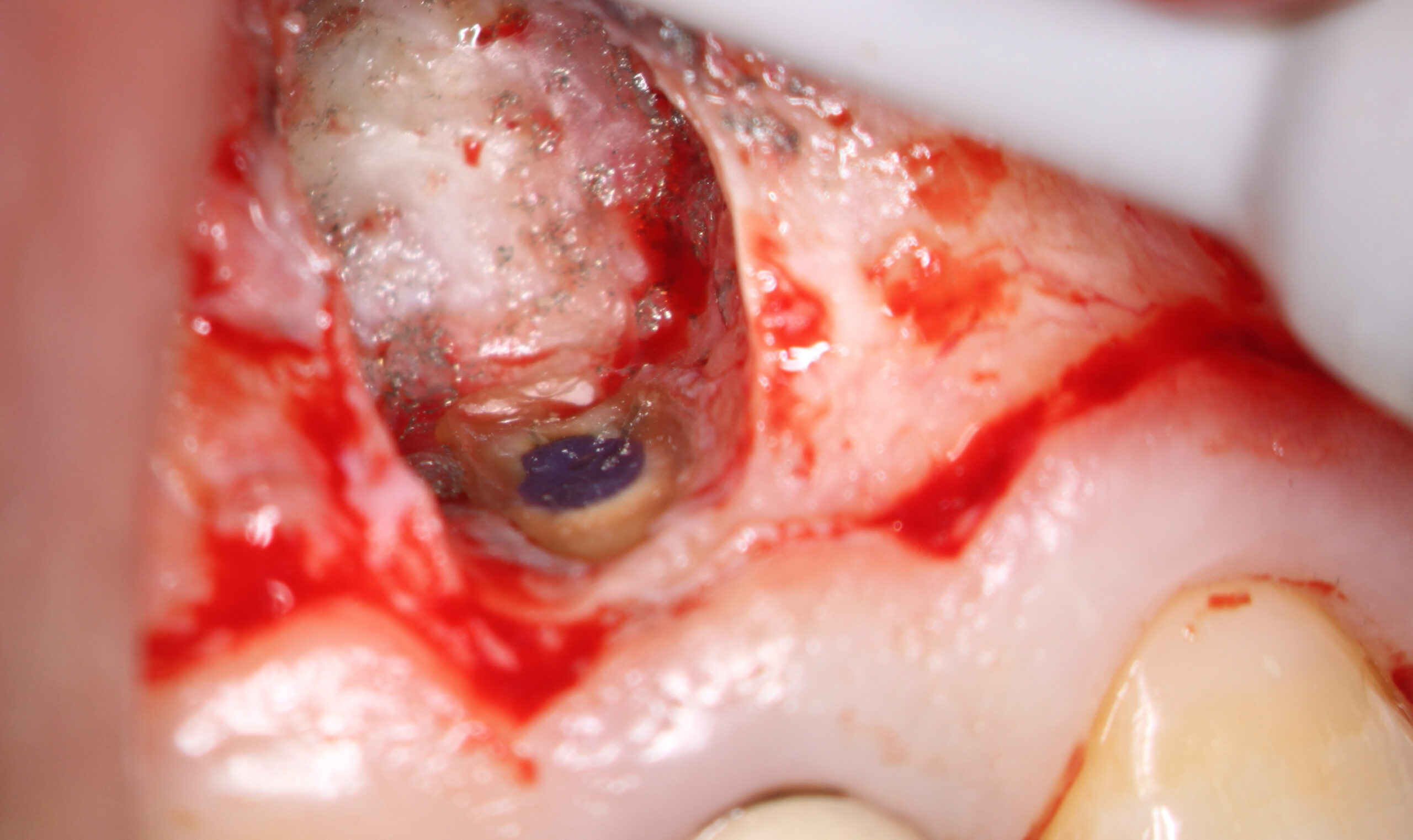
In this case I was unsure as to how well a minimal thickness of MTA cement would seal so I chose to use a flowable composite- Ultradent Permaflow purple . This is the same material I use for orifice bonds. The root was etched, rinsed and a bonding agent was placed and the flowable composite was placed over the retro preparation site. At that time of resection, I noticed a small stained vertical fracture (white arrow) on the palatal side of the root but since we were already committed to doing the surgery, I felt it would be best that we continue to completion and see what kind of results we could get over the long term.
The patient was brought back for suture removal and the area appeared to be healing very well.


The patient was then brought back at six months post op at which time the soft tissues looked perfectly normal and radiographic images showed that bone fill was proceeding normally. I was reasonably optimistic at this point but had some concerns regarding the long term viability of the tooth, considering the crown root ratio and the previous fracture that I had seen during the surgery. The patient refused to come in for further recalls and we were unable to examine the tooth either clinically or radiographically at 1 or 2 years postop .

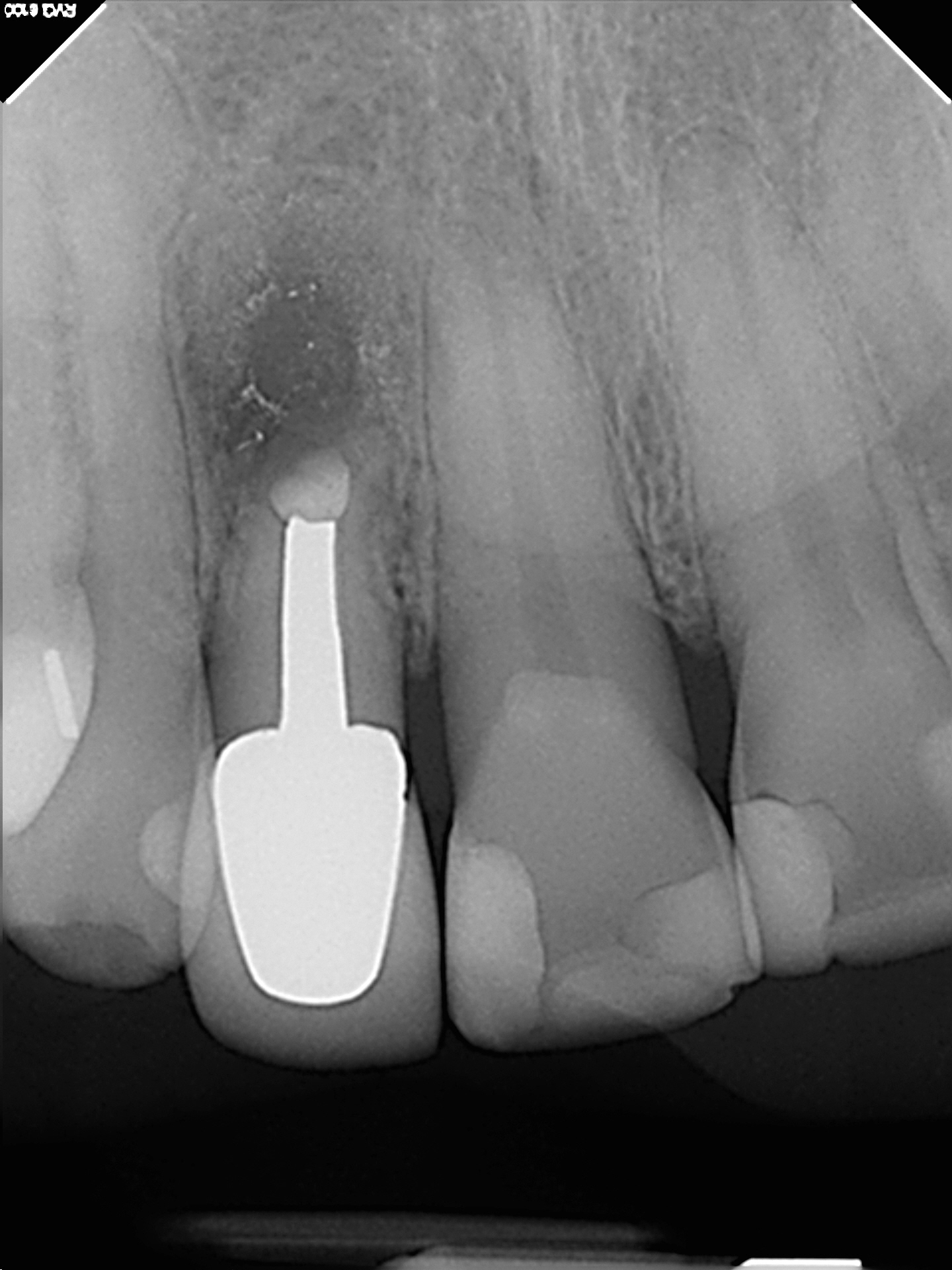
In August of 2021 the referring dentist referred the patient because of the presence of a persistent draining buccal sinus at the apex of this tooth. They enclosed a radiograph and clinical photo which showed that a fragment of the apical portion root had broken off on the distal aspect. This was likely associated with the previous fracture line that I had seen during the surgery.
The tooth will now require extraction and replacement with an implant.
Considering it’s compromised nature, we got about eight years of service out of this tooth although it had both a previous surgery and presence of a fracture.


In retrospect, when I saw the fracture during the surgery, I could have recommended immediate extraction, but in the absence of any pocketing (possibly related to a VRF) we elected to try to save the tooth.
Whenever we perform treatment on suboptimal teeth, we must always have a fully informed patient. In this case, although we eventually will lose the tooth:
(1) we kept the tooth from late 2013 until the summer of 2021 and initially got some healing of the area
(2) after treatment there was minimal compromise of the implant site and the patient can have the tooth prosthetically replaced (with a bridge or implant) with minimal bony defect.
