cbCT Helps With Decision Making
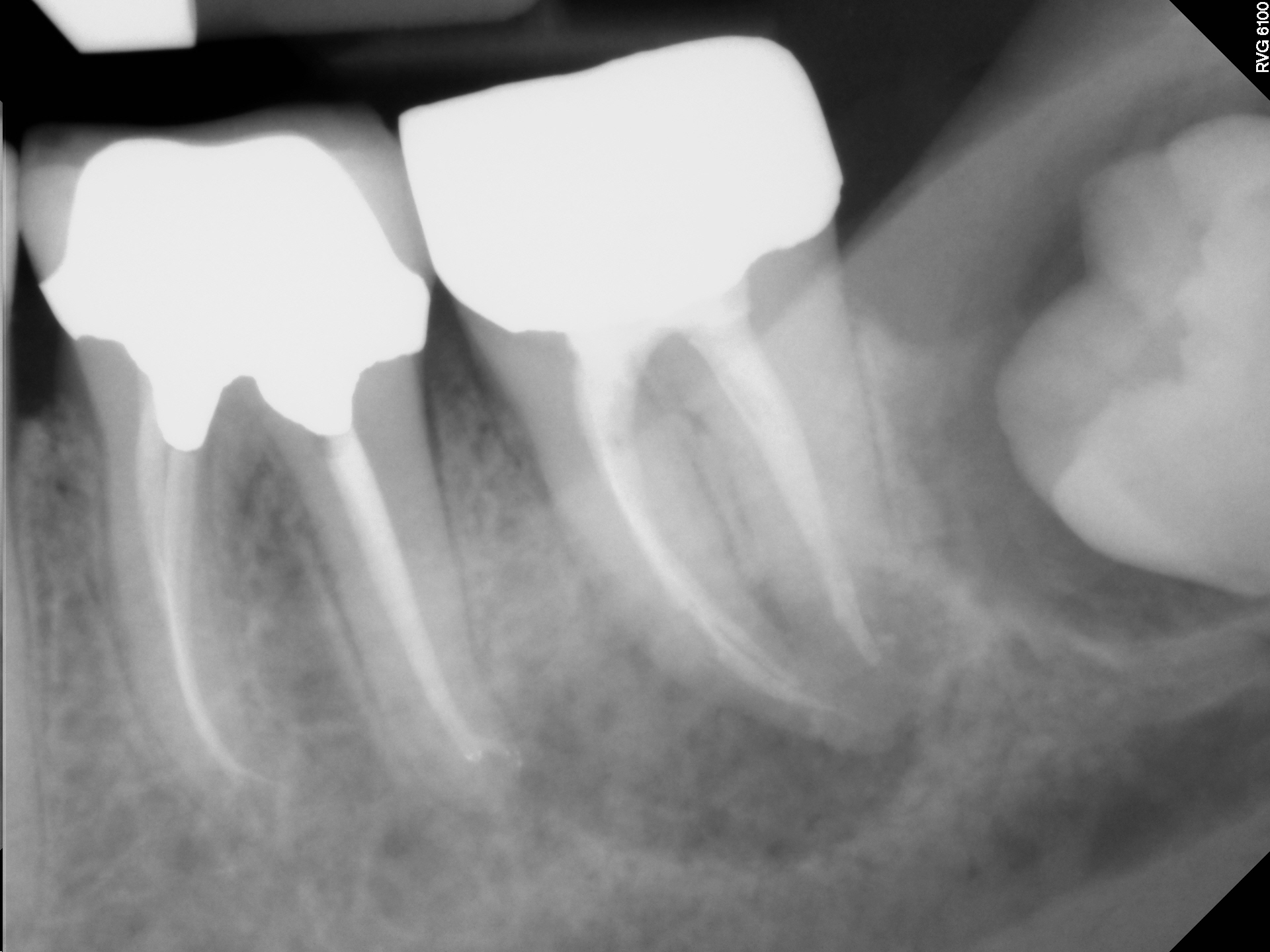
This 60 year old male patient was referred to me for evaluation of the area of tooth #37. The tooth had a history of previous endodontic treatment with full gold Crown restoration. The tooth was percussive sensitive and sensitive to chewing. Distal to this tooth was an impacted tooth #38 with a radiolucent finding associated with this impaction. There was also a radiolucent finding at the mesial root apex of #37. The referring dentist was unsure as to what the source of the problem may be and was unsure as to whether to proceed with extraction of 38 or retreatment of #37.
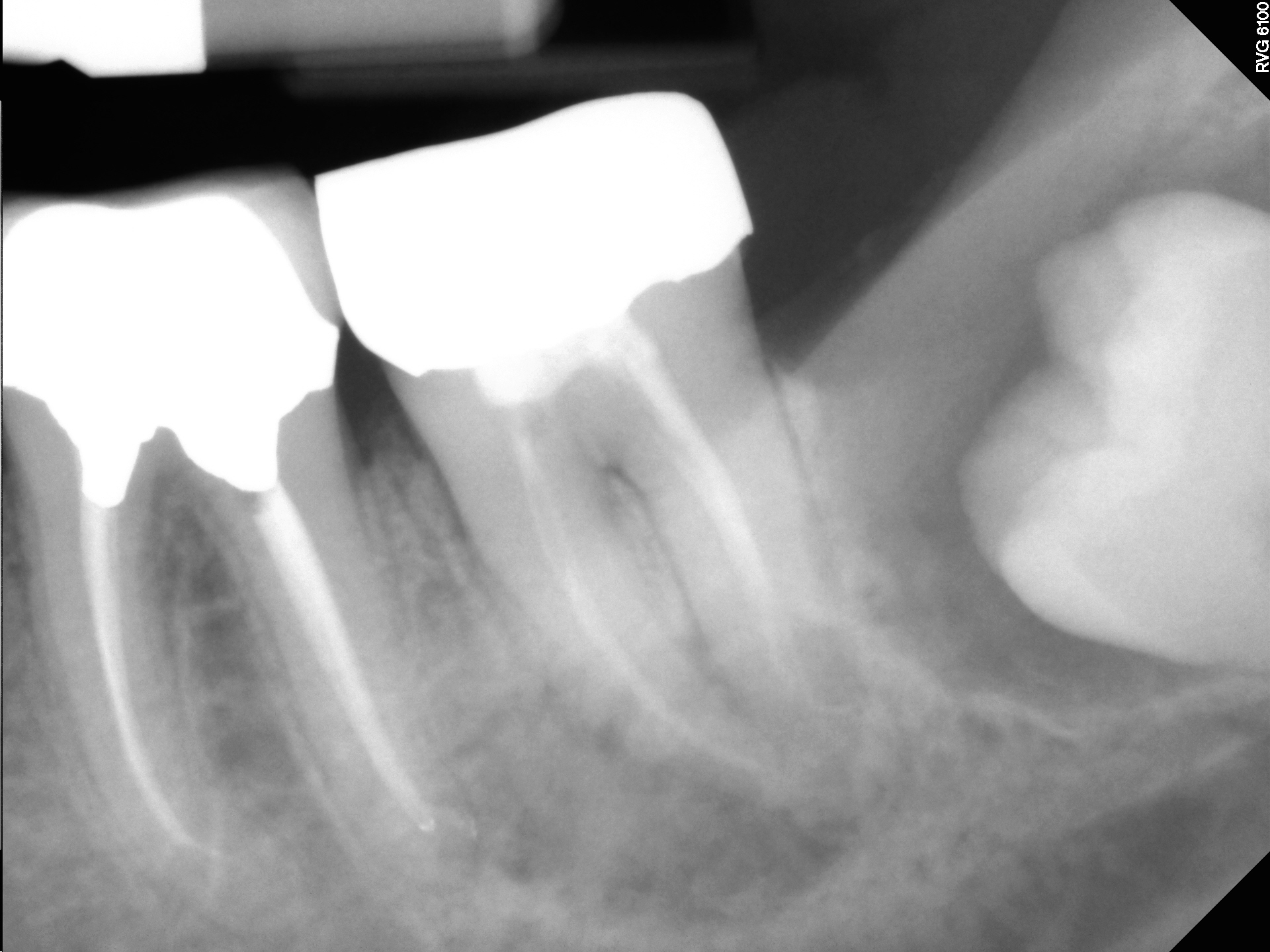


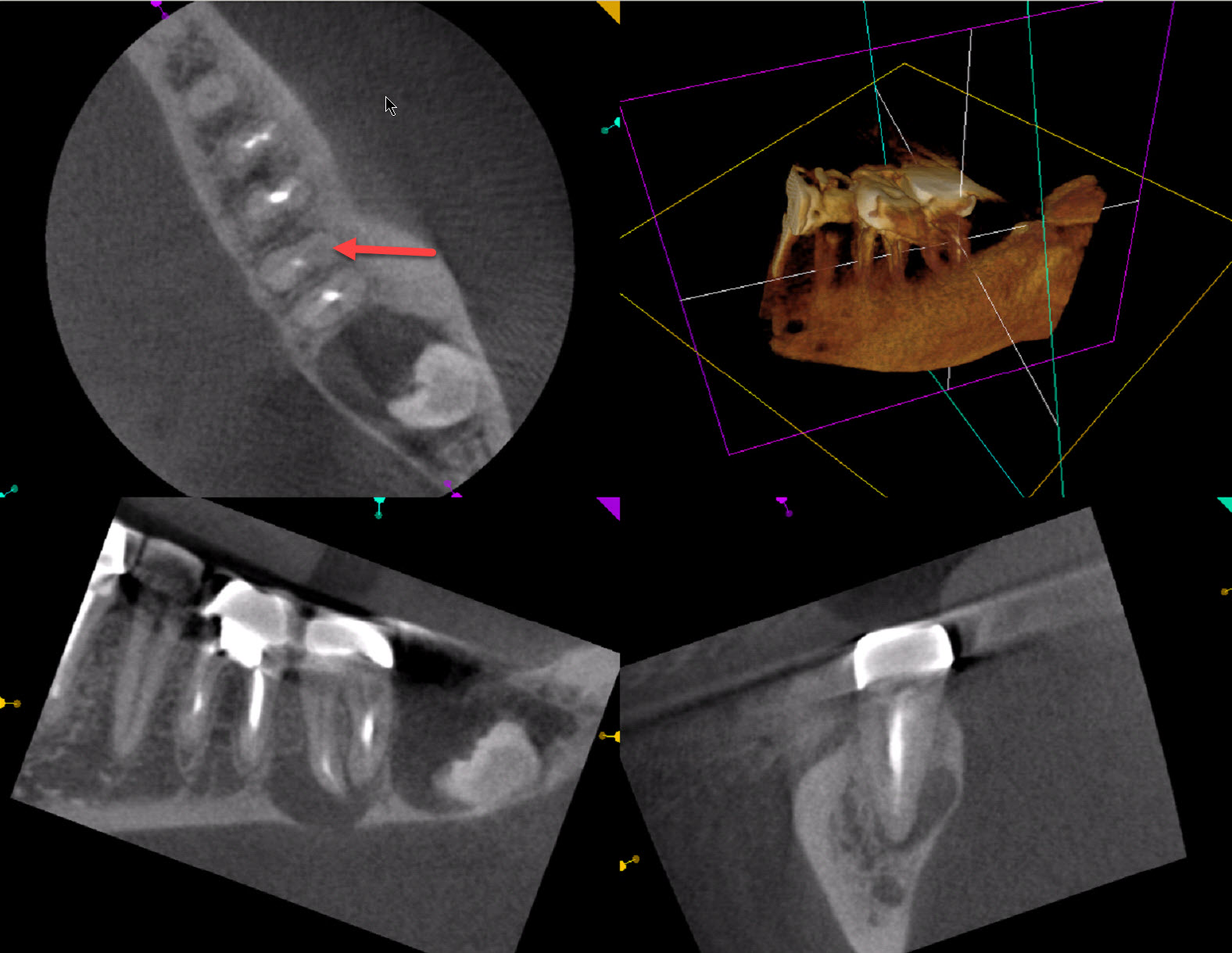
Periodontal probing of the area revealed no abnormal pocketing on the distal aspect of #37. Cone beam tomography revealed persistent radiolucent finding at the mesial root apex of tooth number 37 and an apparent missed canal in the mesial root.
The patient was scheduled for endodontic re treatment of tooth #37 and re evaluation of tooth #38 once re treatment had been completed .
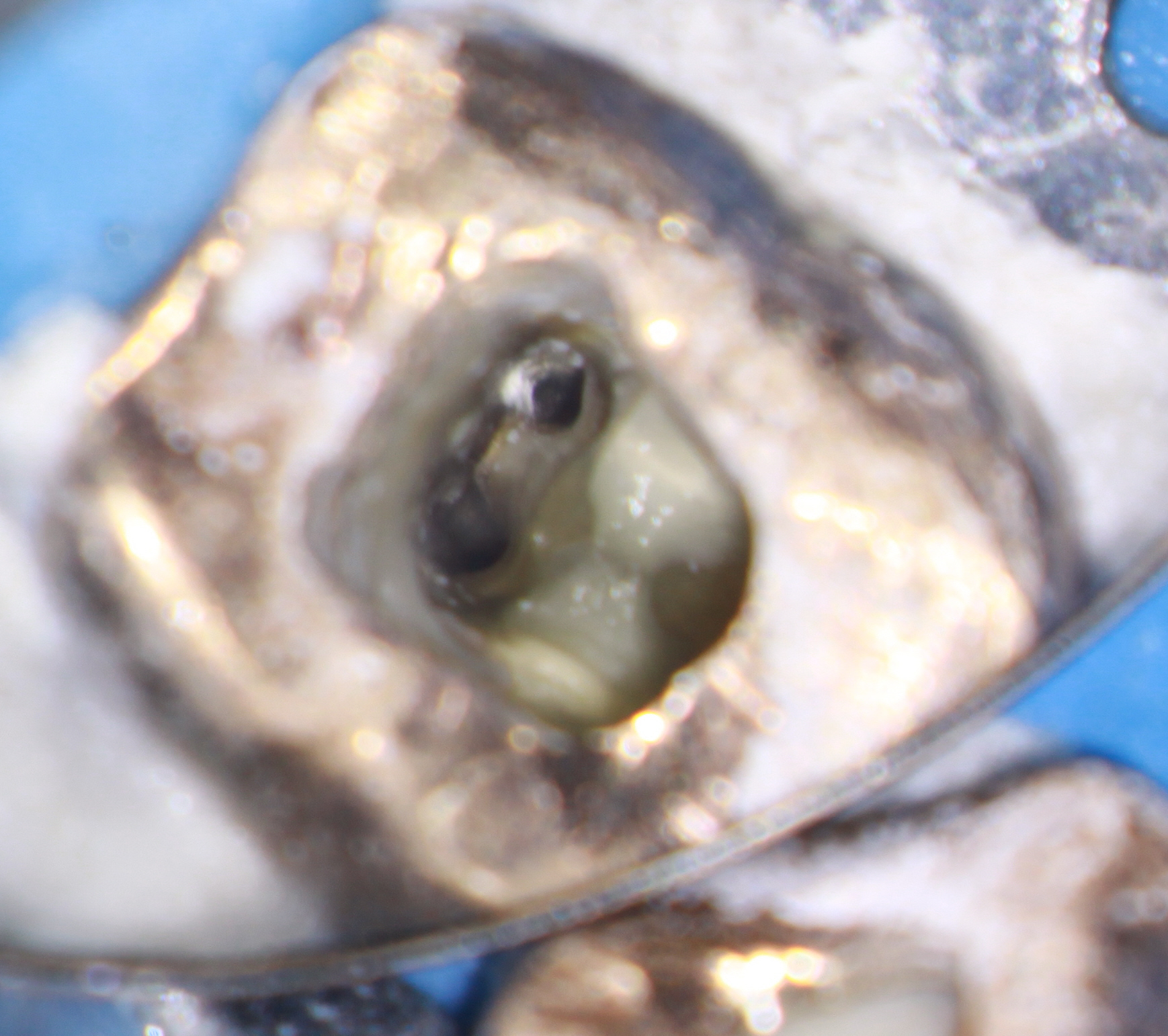
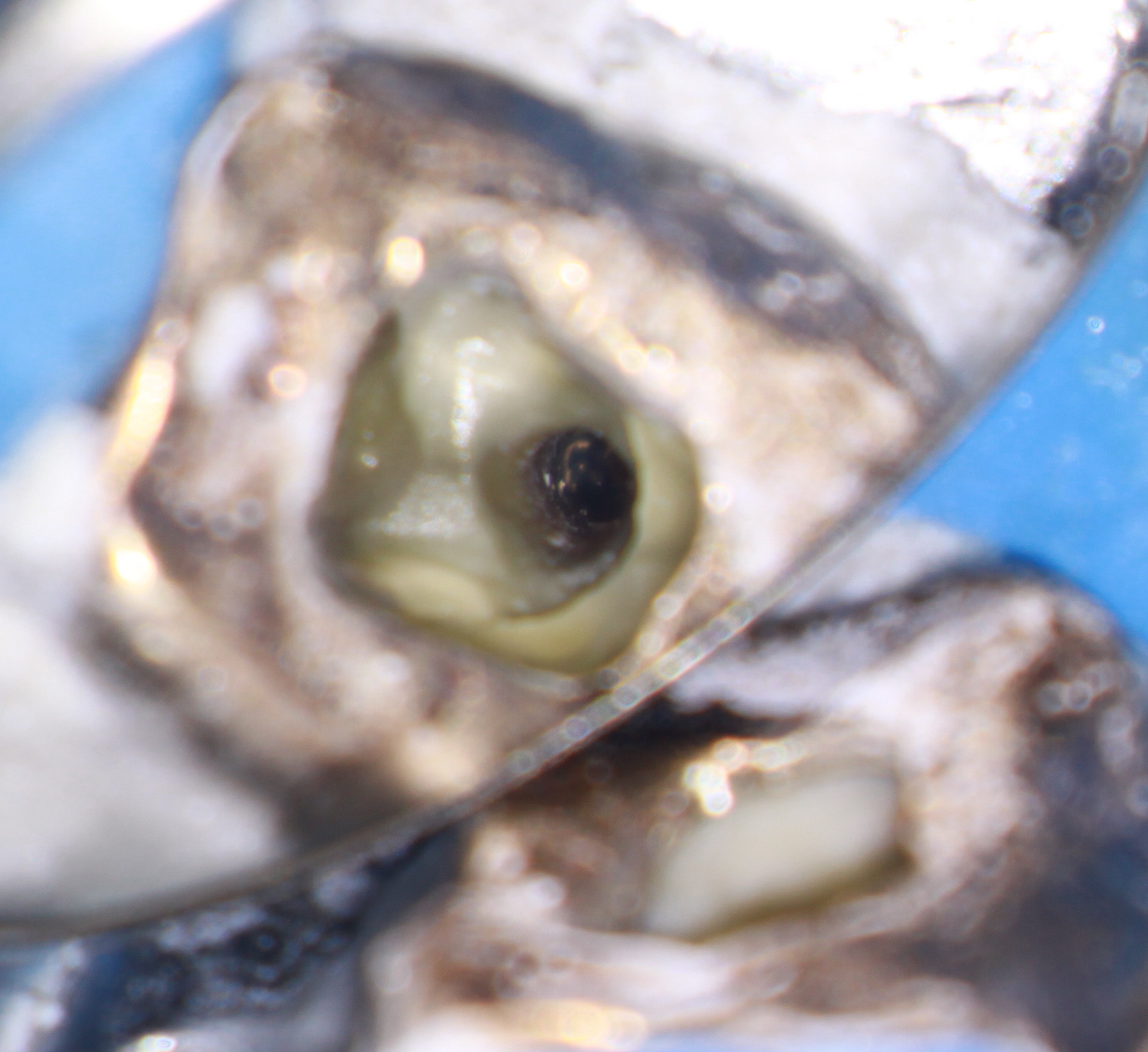
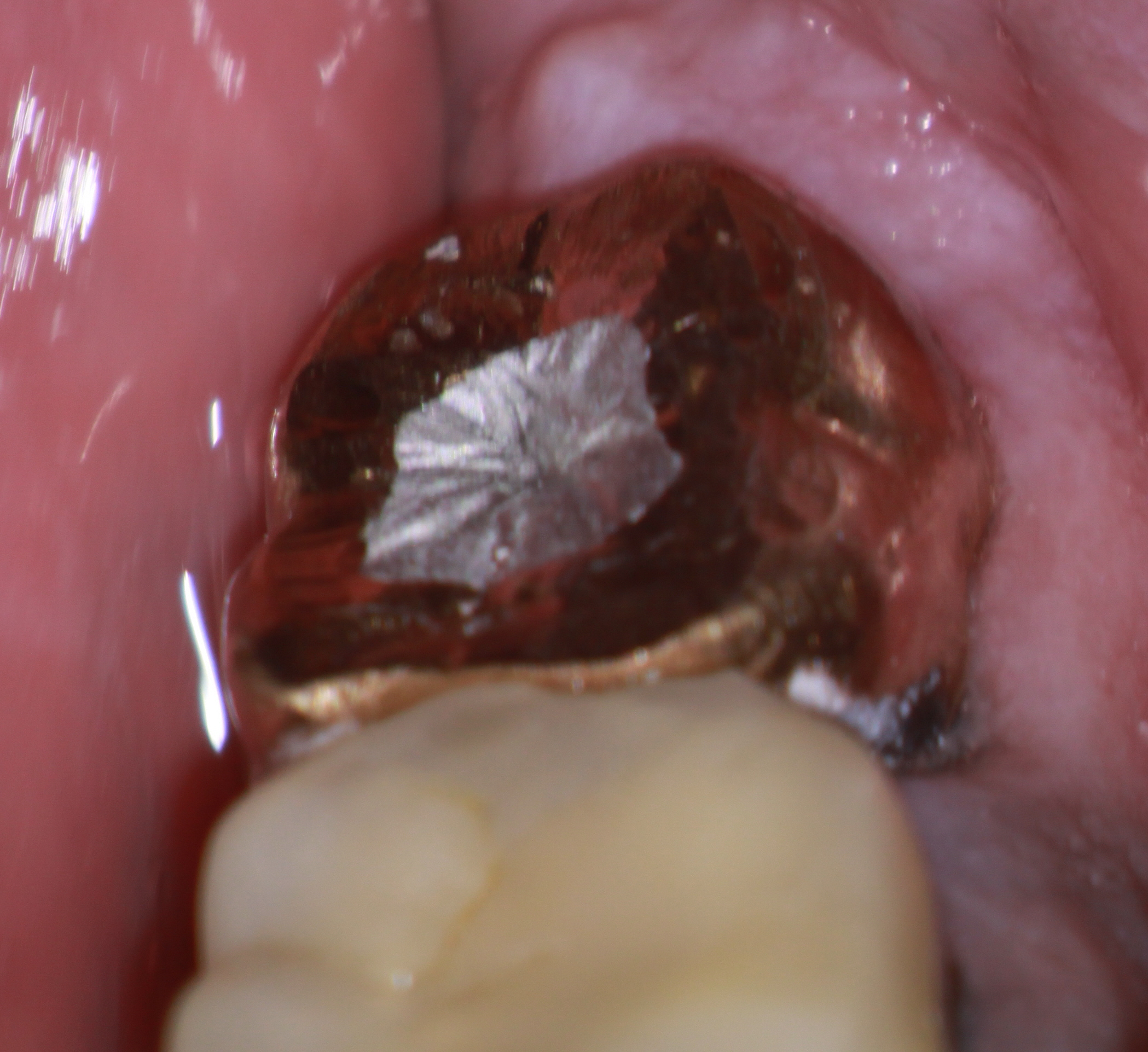
The tooth was accessed , the canals cleaned and shaped and medicated with calcium hydroxide. Approximately 2 weeks later the patient returned asymptomatic and the case was completed and the access closed with amalgam.

Unfortunately, the patient refused attempts at recall but the referring dentist said the patient was asymptomatic and had not preceded with extraction of #38.
This case is interesting in The timing and sequence of treatment that could have been proposed. Having established that tooth #37 was the source of the patient’s current complaint, it seemed logical that we solve the endodontic problem first. However, in order for us to do this we had to inform the patient of the impacted wisdom tooth and the possible detrimental effect that removing it could have on the adjacent supporting bone adjacent re treatment, should removal of this wisdom tooth be deemed necessary. It could compromise the distal support for the retreated tooth. Once the patient was given all this information, he chose not to have the wisdom tooth extracted and agreed to have us proceed with re treatment of the second molar.
The information given to us by the cone beam tomography allowed us to present several options to the patient. I felt somewhat confident in the fact that along with the percussion sensitivity and the apparently untreated canal in #37, we could predictably resolve the patients current complaint. However I was unsure as to whether extraction of the adjacent impacted 3rd molar might have an effect on whether we could retain #37 , due to other factors. Given the above information, the patient chose to have #37 retreated and chose to leave #38 without further treatment.
